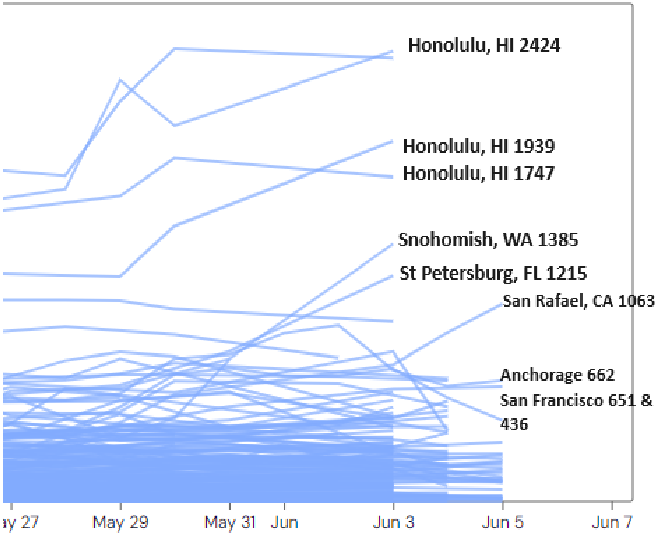
Wastewater levels of SARS-CoV-2 are extremely high in Hawaii now. Per WastewaterSCAN, nationally, the highest levels of virus are in Honolulu (2424 PMMoV); Snohomish, Washington (1385 PMMoV); St. Petersburg, Florida (1215 PMMoV); and San Rafael, California (1063 PMMoV).
From Wastewater SCAN: https://data.wastewaterscan.org/
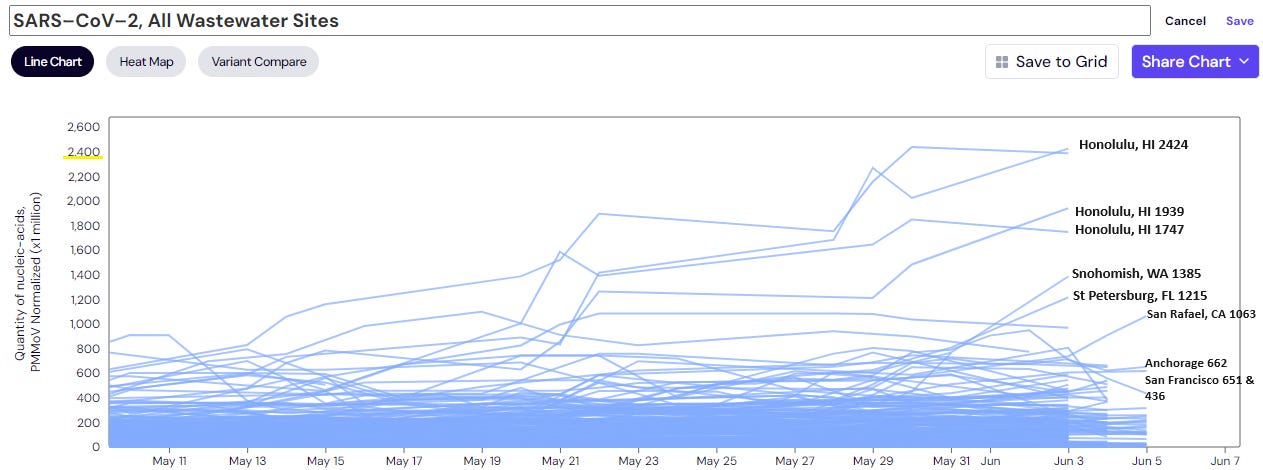
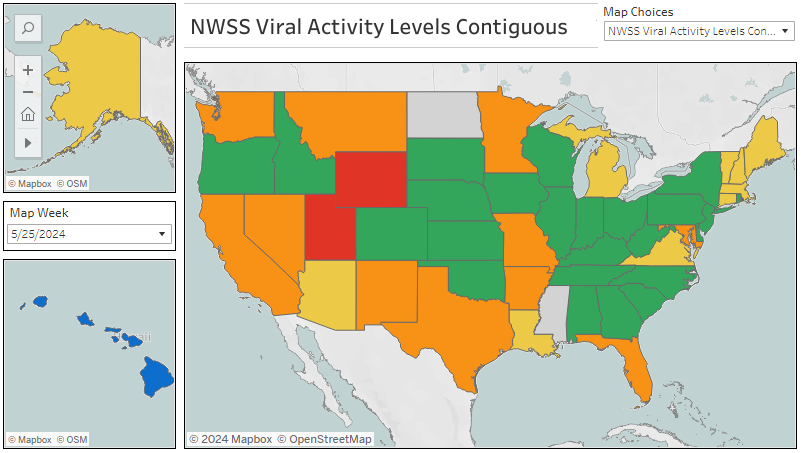
In the Bay Area, Sunnyvale, California is at 571 PMMoV of COVID virus in wastewater which is the second highest level (581 PMMoV) there since 2021 when WastewaterSCAN began reporting.
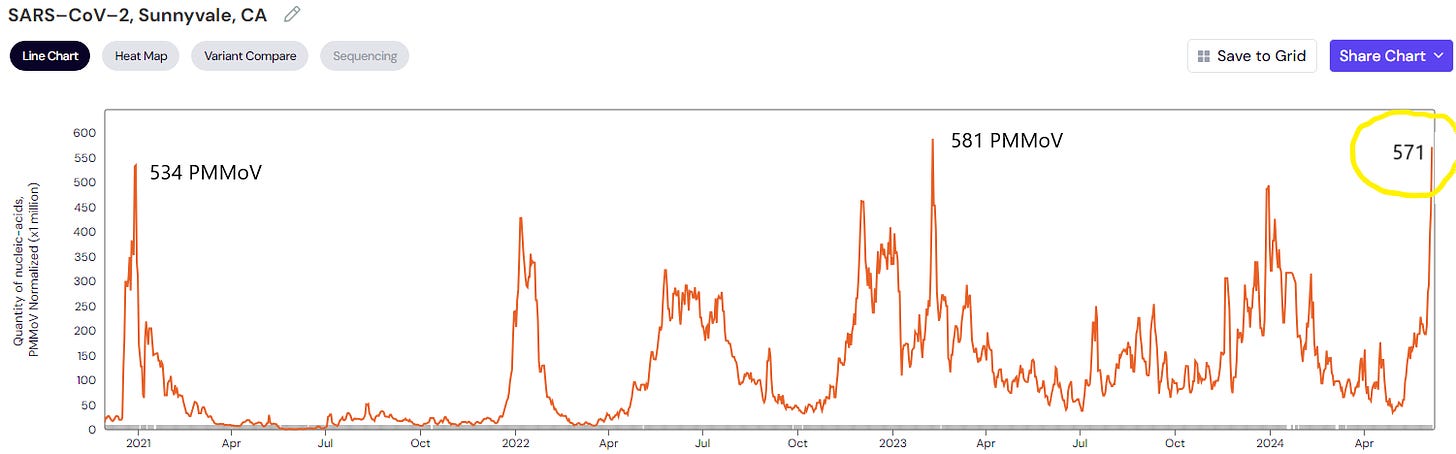
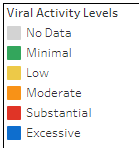
Nationally, wastewater levels of COVID reported as “LOW” by the CDC, but WastewaterSCAN labels them as “MEDIUM”. Sara Anne Willette’s analysis shows that Hawaii’s wastewater COVID level is “Excessive” and that Wyoming and Utah wastewater levels are “Substantial”. Per JP Weiland, about every 1 in 168 people is infected with COVID now in the United States, although levels vary by state and even by county. Given the exceptionally high viral levels in Hawaii, I would estimate that 1 in every 20 people in the Aloha state has COVID now.
Hawaii’s levels are super HIGH (“Excessive” per Sara Anne Willette)
Wyoming, Utah are substantial
Many others are moderate now
National SARS-CoV-2 data from Sara Anne Willette: https://iowacovid19tracker.org/
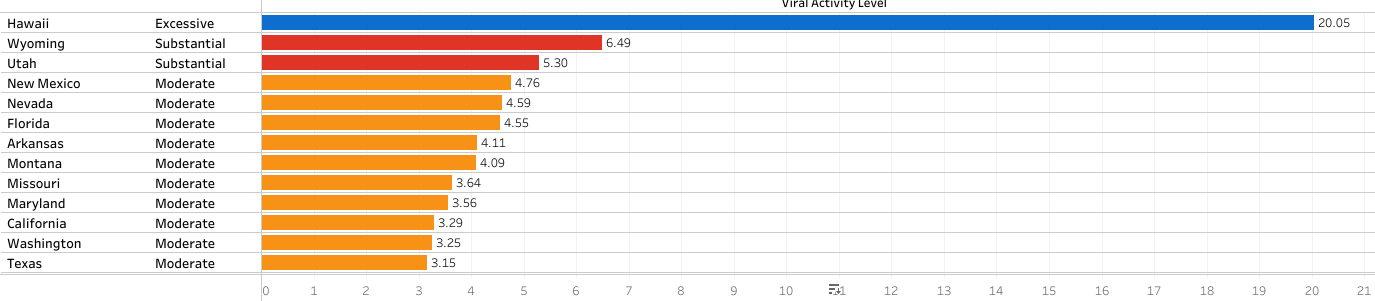
Variants
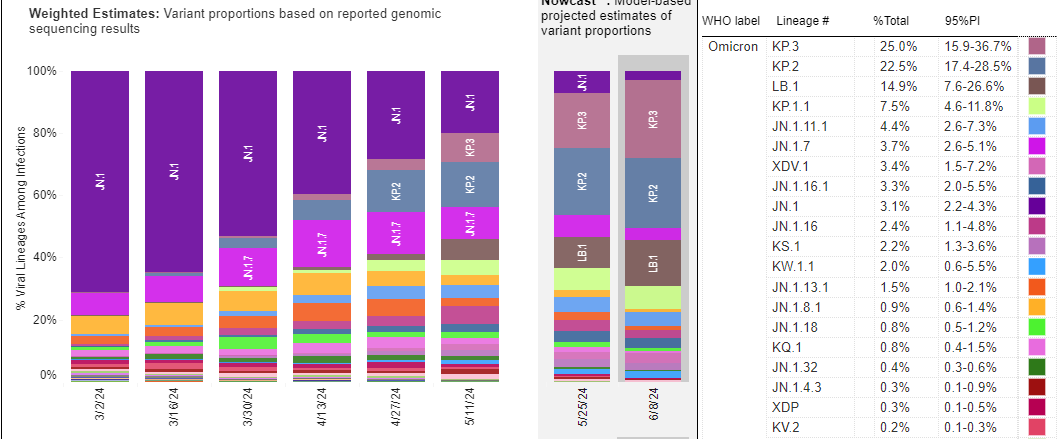
KP.3 (JN.1 + F456L + Q493E), a “FLuQE” variant, is immune evasive and has outcompeted KP.2 in the United States. KP.3 is causing a COVID wave in Australia now.
LB.1 (JN.1 + S31del + F456L + R346T), a “deFLiRT” variant, is also increasing in U.S. COVID cases. In the past with XBB variants, the F456L mutation in the spike protein gave a significant advantage.
From CDC US Variant tracker: https://covid.cdc.gov/covid-data-tracker/#variant-proportions
According to Yunlong Cao, “KP.3 is starting to outcompete KP.2. Its unique Q493E mutation brings some critical features:
1) KP.3 has higher ACE2 binding affinity than KP.2.
2) KP.3 is more immune evasive. KP.3 +31del (KP.3.1.1) is the most.
3) KP.3 is especially good at evading Class 1 antibodies.”
Because of its unique Q493E mutation, Yunlong Cao’s testing shows that KP.3 can evade neutralizing antibodies from JN.1 infection. Therefore, he states “we would expect KP.3 and KP.2 to show substantial immune evasion even with JN.1 mRNA boosters.” He therefore recommended that the new mRNA vaccines for the Fall be based on either KP.3 or KP.2.
Kei Sato’s lab found that “deFLiRT” variants LB.1 and KP.2.3 are more infectious than KP.2 and KP.3 in pseudovirus infection studies. He predicts that “LB.1 and KP.2.3 have the potential to be predominant variants in the near future, due to higher infectivity and increased immune evasion.”
On June 5th, the Vaccines and Related Biological Products Advisory Committee (VRBPAC) from the FDA met to discuss the upcoming formulation of the 2024-2025 COVID vaccine. They decided to base the Fall vaccine on JN.1. Here is data from each of the three vaccine makers that was presented at this meeting:
According to CIDRAP, after the VRBPAC vote for JN.1, "FDA officials asked advisory group members to weigh in on whether to select a specific JN.1 lineage, such as KP.2." But, they chose to stick with JN.1 because Novavax had already started working on it. Protein vaccines like Novavax take about 6 months to make. Several committee members also said that they did not want to be "chasing variants."
Yunlong Cao’s data showed that “we would expect KP.3 and KP.2 to show substantial immune evasion even with JN.1 mRNA boosters”. Eric Topol tweeted that “The new Covid booster planned for September is directed vs JN.1. It's already a mismatch where we are now, and soon will be, with KP.3 becoming dominant.” Other scientists (JP Weiland, Ryan Hisner) tweeted that it would have been better to make the Fall vaccine against a JN.1 subvariant with a F456L mutation.
COVID and Cancer:
The Washington Post reported that in 2021, Dr. Patel’s oncology group noted seven cases of cholangiocarcinoma, a rare and lethal cancer of the bile ducts. They also saw 15 patients who presented with several different types of cancer at the same time and other cases of rare cancers. They wondered if COVID infections could be linked to these unexpected cancers. Other viruses are associated with cancer. HPV causes cervical cancer, EBV can induce Burkitt's Lymphoma, and Hepatitis B can lead to liver cancer.
Regarding the rare cholangiocarcinoma cases, ironically in 2023, Mike Hoerger was reviewing Ziyad Al-Aly’s data which showed an increase in some chronic diseases 2 years after COVID infection. Mike noted that the risk of cholangitis (bile duct inflammation) in the paper was quite high and tweeted “I found it striking the level of elevated risk to the bile duct from reinfections and also suspect we will see a rise in bile duct cancer.” The findings of cholangiocarcinoma noted anecdotally by the Patel oncology group are most likely due to chance, but this would be worth following over time.
Testing and Treatment
Is it COVID or is it the Flu? Eric Feigl-Ding tweeted a link to an at home multiplex rapid test that can detect COVID, as well as Influenza A and Influenza B. He gave a promo code for a 20% discount on these pricey tests. In California, clinics that offer free COVID tests can be found on the California My Turn website. The Pfizer PAXCESS site helps people with Medicare, Medicaid or people who are uninsured to get Paxlovid for free and may reimburse the co-pay costs of Paxlovid for those who have private health insurance.
Long COVID
In 2022, the Social Security Administration requested that the National Academies review the current status of diagnosis, treatment, and prognosis of Long COVID. A committee of experts from different medical specialties met seven times under the direction of the National Academies of Science, Engineering and Medicine (NASEM) to review the scientific literature with an emphasis on how Long COVID affects normal functioning and disability. They found that “Long COVID is real” and that the Social Security Administration “does not provide sufficient guidance for assessing functional status or weighing severity.” STAT news and the New York Times each wrote great explainer articles on the NASEM findings.
The NASEM report is almost 250 pages long. Here are some key points from the NASEM document and from STAT news:
5.3% of U.S. adults — 13.7 million people have Long COVID.
Long COVID is most likely a long-term chronic illness for which there are no treatments at this time.
Prognosis: While many of the more than 200 Long COVID symptoms “generally improve over time,” recovery tends to plateau at 6 to 12 months after the initial COVID infection. Full recovery at one year only happens in about 22% of people with Long COVID at this time.
Trials: The NASEM committee discussed enhanced external counter pulsation (EECP) to help Long COVID patients with endothelial dysfunction in the heart blood vessels. EECP is not recommended for someone who is hypercoagulable though. The team also discussed Cognitive behavioral therapy (CBT), Rintatolimod (Ampligen) and Metformin clinical trials that are under way.
Pediatrics: Children and teens can get LC. Most common symptoms in this age group are fatigue and headache. Psychiatric disorders such as anxiety can be common too. Type I diabetes is increased after COVID infection in children and Type II diabetes is increased in adults who have had COVID.
In adults, disabling fatigue, post-exertional malaise (PEM), cognitive dysfunction and autonomic dysfunction are common and can be incapacitating.
87% of Long COVID patients have PEM. “PEM is when minor effort — physical or mental — can wipe out a person’s energy and cause a worsening of symptoms in the days following.”
24% of people with Long COVID have cognitive dysfunction. “Cognitive impairment includes difficulties with thinking, memory, attention, processing information quickly, language, and executive functions like problem-solving or multitasking.”
At least 25% to 66% of people with Long COVID have autonomic dysfunction which can include POTS (postural orthostatic tachycardia syndrome). Symptoms can include elevated heart rate, difficulties with balance, lightheadedness, brain fog, nausea and the inability to stand or be upright.
40% – 70% of long Covid patients meet the criteria for ME/CFS and 39% for fibromyalgia, a chronic pain syndrome.
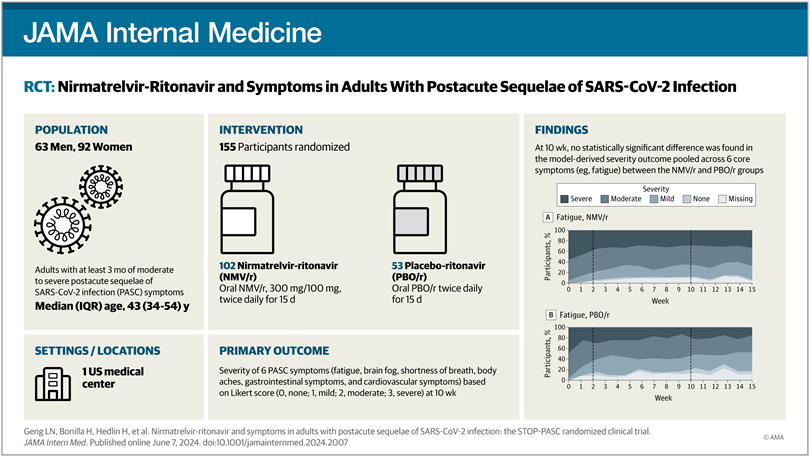
Paxlovid trial for Long COVID
A group from Stanford reported in JAMA on their randomized clinical trial of 15 days of Paxlovid vs. placebo for Long COVID. In this study, 102 patients with Long COVID received Paxlovid and 53 Long COVID patients were given placebo. They found that “a 15-day course of nirmatrelvir-ritonavir [Paxlovid] in a mostly vaccinated study cohort was generally safe, but did not show significant benefit in improving fatigue, brain fog, body aches, cardiovascular symptoms, shortness of breath, or gastrointestinal symptoms."
From: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2819901
Michael Peluso tweeted about the Stanford Paxlovid study commenting that the study was “beautifully done” and because it was a small trial, it may not have been able to show which Long COVID patients that may benefit. Long COVID is a very heterogeneous disease and we do not know yet which patients may improve with a longer course of Paxlovid or from monoclonal antibodies or immune modulators. He agreed with the authors who said, "The landscape of PASC research is dynamic. Smaller studies that are more focused and agile can scout the terrain ahead of larger and more definitive studies."
In a keynote address at the Unite To Fight conference last month, Johan Van Weyenbergh reviewed data from an ongoing study in his clinic. This data has not yet been published. In the short video clip from his talk, many Long COVID patients in his clinic did not improve with Paxlovid for 15 days, but some did. Going forward, we will need to figure out which patients this therapy can benefit. They found a 32% decrease in Long COVID symptoms overall, but some patients worsened, many had no relief from Paxlovid and some improved. His entire talk is available here.
Another study from Stanley Perlman’s lab shows that while early treatment with Paxlovid reduced viral titers and improved lung inflammation, Paxlovid failed to prevent neurological abnormalities in mice. Chronic inflammation associated with increased proinflammatory cytokines in areas of the brain led to persistent microglia activation and neurodegenerative changes associated with SARS-CoV-2 infection.
The BBC reported on how studying concussions can offer insights into Long COVID neurologic problems. In humans, post-concussion traumatic brain injury (TBI) shows similar patterns of fatigue, sleep disturbances, light and noise sensitivity, exercise intolerance and problems with memory and concentration as Long COVID. University of Denver researchers noted that Long COVID patients, like post-concussion patients, have difficulty tracking eye movements and their “balance and spatial reasoning examinations also suggested that the [Long COVID] patients had effectively experienced a traumatic injury to the brain." The article also discussed how some ME/CFS patients can have weakness in the ligaments that hold the skull in place over the neck and this can put pressure on the brainstem which may lead to autonomic dysfunction. Herbert Renz-Polster recommended using ultrahigh-field (UHF) MRI scanning to evaluate the neck in people with ME/CFS.
In acute COVID infection, cytokine storm with high levels of interferon‐γ (IFN‐γ), interferon-β (IFN-β), interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) can occur. This triggers the IDO-1 enzyme, which starts the breakdown of tryptophan in the kynurenine pathway which can lead to some neurotoxic and immunosuppressive substances. Authors noted elevated kynurenine pathway metabolites are seen in acute COVID infection and in Long COVID, especially in people with cognitive impairment. They concluded, "it is likely that the kynurenine pathway involvement is significant in SARS-CoV-2 pathogenesis, especially neurologically."
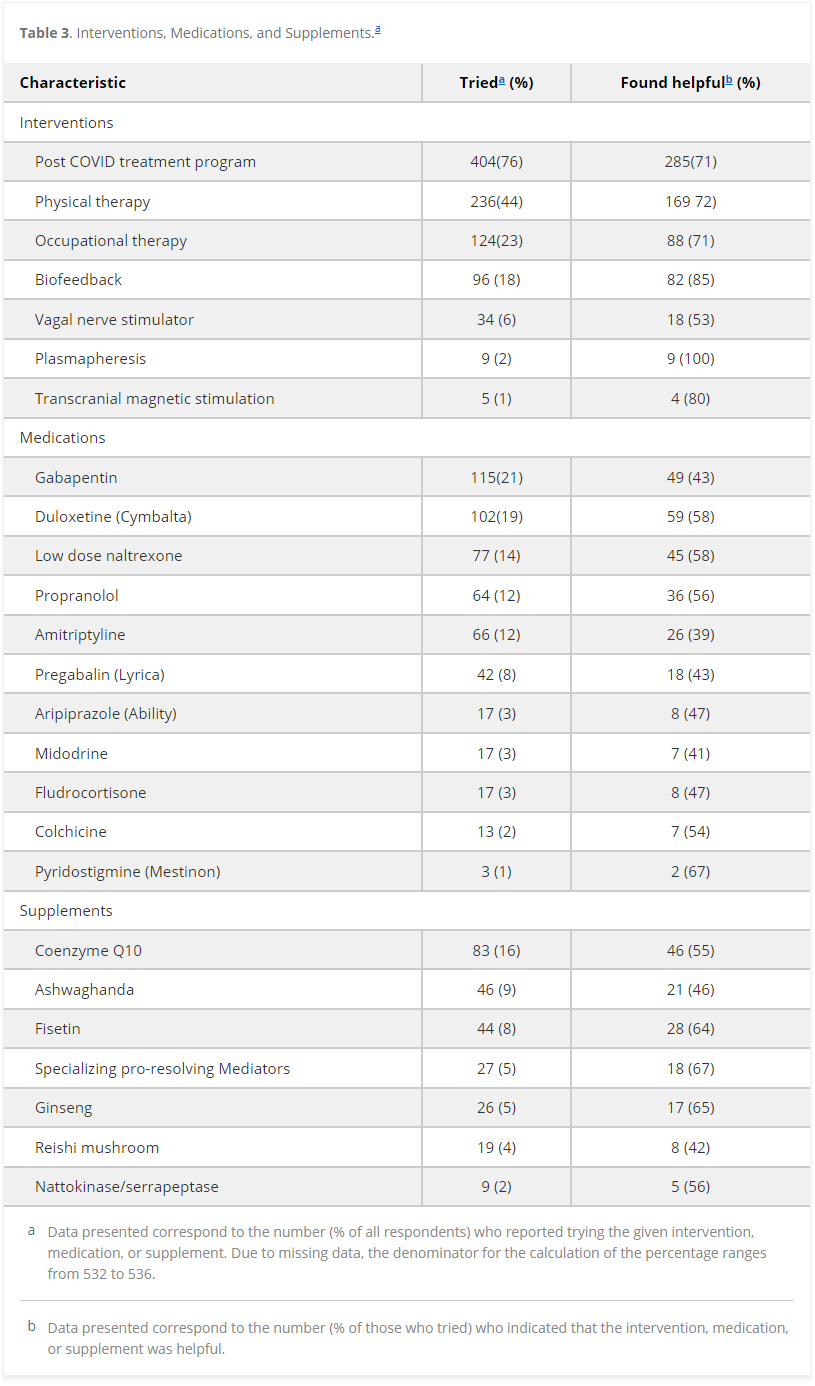
The Mayo Clinic Post-COVID clinic shared a survey of 536 people with Long COVID who were followed longitudinally by their clinic. The questionnaire showed that while Long COVID symptoms were often improved from initial visit until the time of the survey, only 4.5% of patients rated their symptoms as low, thus indicating that there were few people who had a full recovery in this group. “The patients rated numerous interventions as being helpful, including low-dose naltrexone (45/77; 58%), vagal nerve stimulation (18/34; 53%), and fisetin (28/44; 64%).”
Table 3 from https://journals.sagepub.com/doi/10.1177/21501319241258671
A mega-review of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) came out this week, but I haven’t had time to read it completely yet. I wanted to include it, so that others can start reading it now.
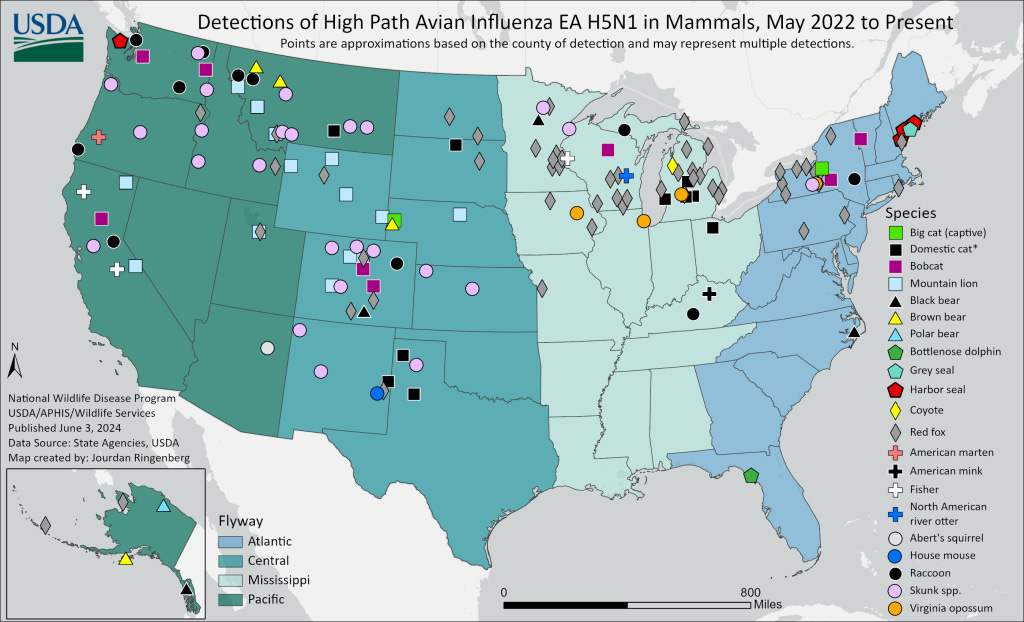
H5N1
On June 4, the USDA reported that 11 house mice from New Mexico had been infected with the H5N1 Avian flu virus. According to virologist Florian Krammer, “wild type mice are [usually] pretty refractory to influenza virus infection.” The samples from the 11 mice were collected on May 8 and 9, but the H5N1 virus was not confirmed until May 24 and was not reported until June 4 on the USDA website. No sequencing data on the virus in the infected house mice has been released. Virologist Rick Bright tweeted about the need for H5N1 viral sequencing of animals, human workers and milk and meat products.
From the USDA: Map of HPAI in mammals since 2022 https://www.aphis.usda.gov/livestock-poultry-disease/avian/avian-influenza/hpai-detections/mammals
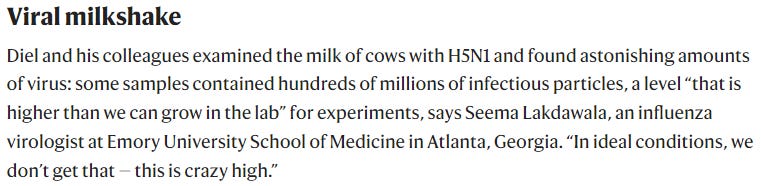
Nature magazine had a concerning article this week on “huge amounts of bird-flu virus found in raw milk of infected cows”. The author, Max Kozlov, spoke of the “astonishing amount of H5N1” found in milk and that the milking process, which can be somewhat messy, appears to be a route of spread from cow-to-cow and from cow-to-human. Therefore, finding ways to disinfect the milking equipment between animals may reduce the spread of H5N1 avian flu.
From https://www.nature.com/articles/d41586-024-01624-1
According to the Des Moines Register, an egg facility with 4.2 million chickens and a farm with 103,000 turkeys were infected by H5N1 in the same week in Iowa.
-----------------
To read the entire newsletter, click here.









.jpg)
No comments:
Post a Comment