Covid wastewater doesn't mean what it used to. Fortunately, we've got it figured out.
Relating wastewater levels and hospitalizations.
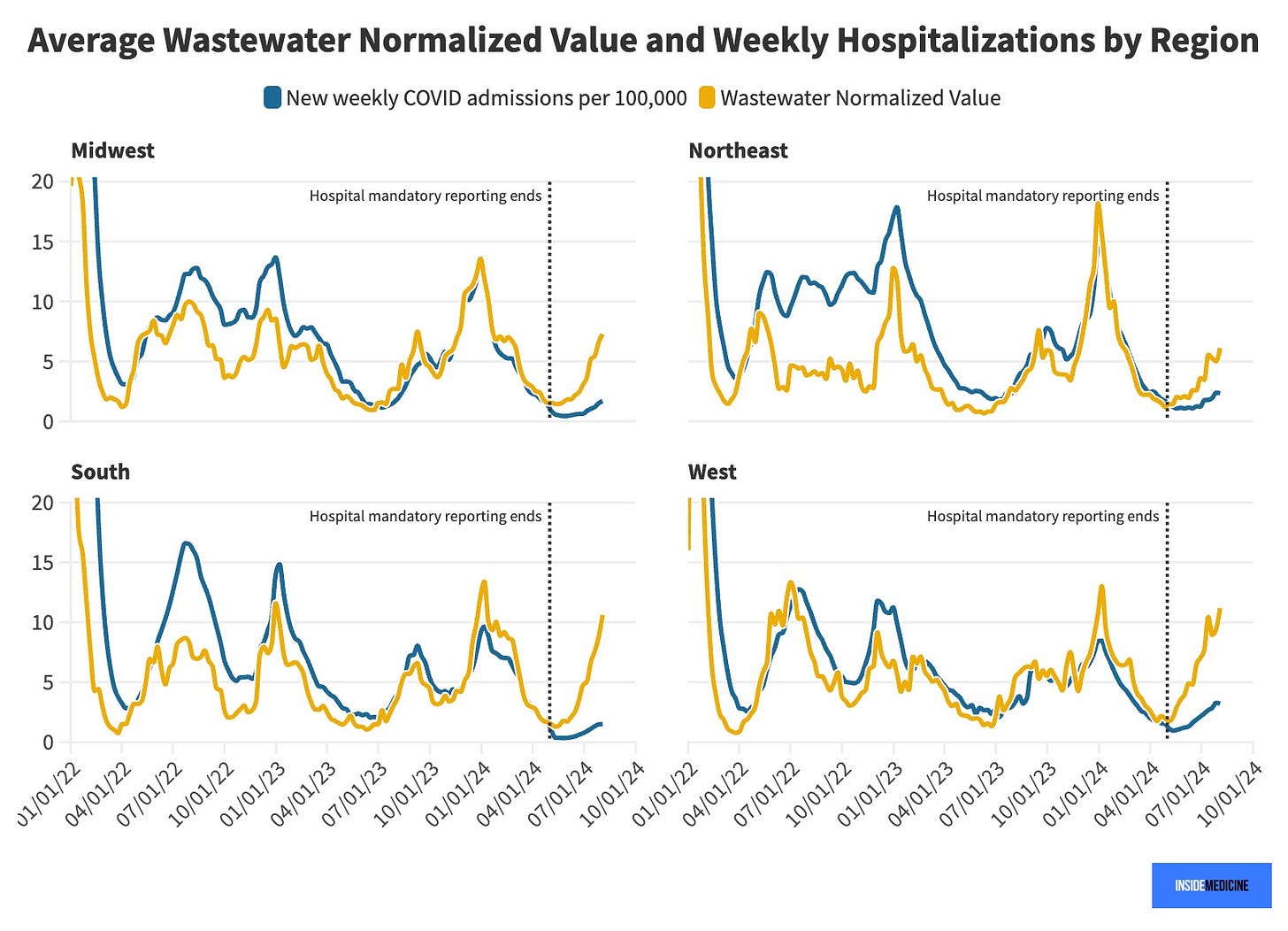
"Going back to early 2022, the relationship between Covid-19 wastewater and hospitalizations in the region was fairly stable for a long time. But, I’ve started to wonder if that relationship has changed recently. So, Inside Medicine’s Benjy Renton looked at the data that powers our Covid-19 metrics dashboard. He graphed weekly Covid-19 wastewater levels and hospitalizations in the four major US regions (with a little conversion to make the lines work on the same Y axis).
"What we found confirmed what I suspected. Take a took…
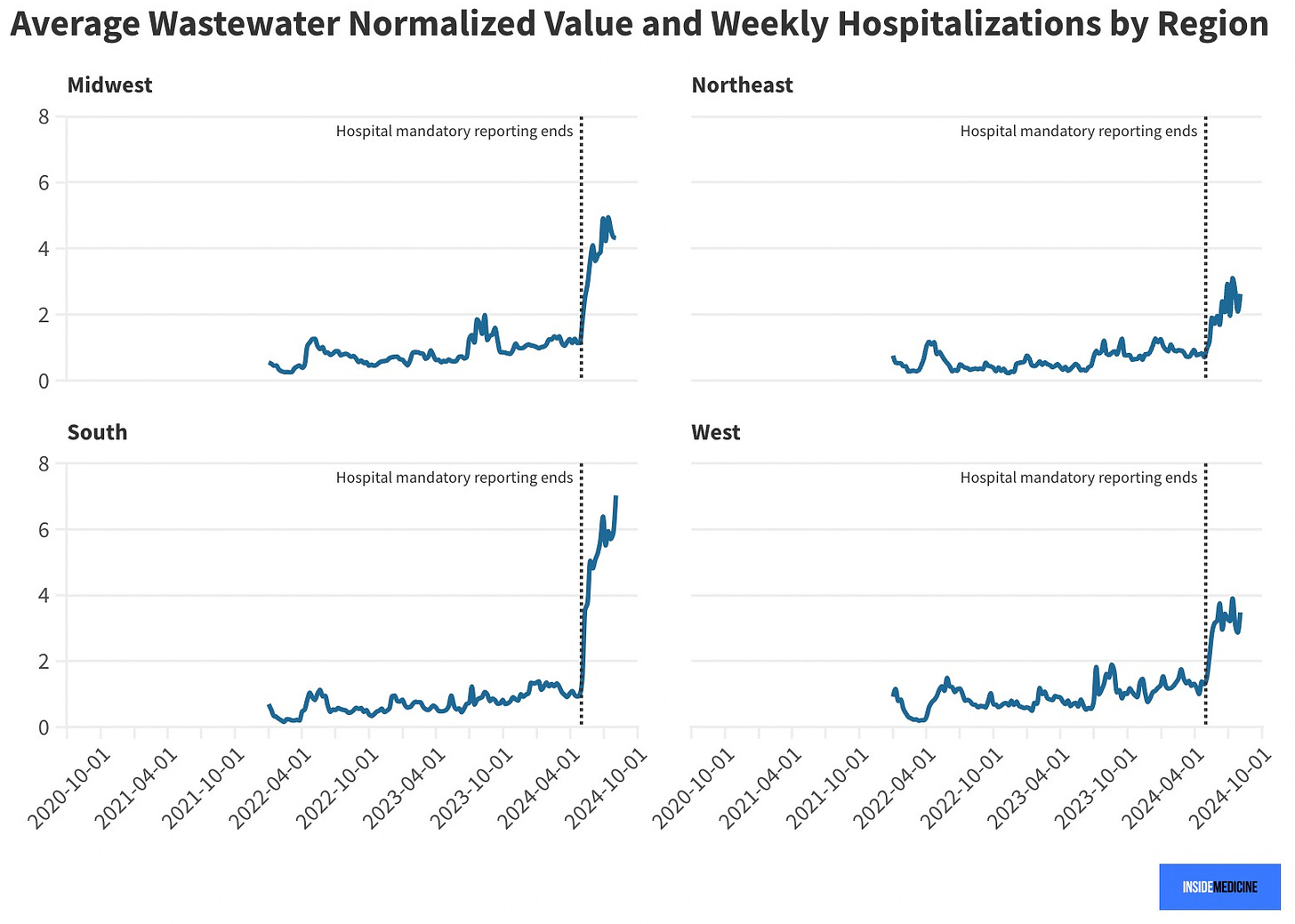
"To me, it appears that from early 2022 until very recently, the relationship between wastewater and hospitalizations was indeed fairly stable. But, after May of 2024 (to the right of the vertical dashed lines) things really uncoupled. To make it more clear, we graphed the ratio of wastewater to hospitalizations over this time. The result confirmed our impressions.
Our interpretation:
"From early 2022 until April 2024, the ratio between wastewater and hospitalizations was more-or-less stable, but slowly increasing. That probably reflected the population gaining immunity over time; that is, the more immune a population is, the more wastewater (i.e., cases) it takes to hospitalize a single person. This makes sense given increasing immunity due to both infections and vaccines. Then, in May of this year, the ratio skyrockets upward. Why? Because this is when hospitals were no longer required to report to the feds when a patient with Covid-19 was admitted to the hospital. As a result, places stopped testing everyone getting hospitalized (and only some continued to report their results). Meanwhile, wastewater reporting is unchanged. The predictable result? The ratio of wastewater to hospitalizations has dramatically increased. Whereas before we could say that it took 1 unit of wastewater (in our graph) to yield 1 hospitalization, now it’s more like 2:1 (Northeast), 4:1 (West), 5:1 (Midwest), and 7:1 (South). This is not surprising given what we know about regional approaches to this virus. The South is much less concerned (and so even doctors there are testing hospitalized patients less) compared to the Northeast.
"The result? The relatively high recent wastewater levels we’ve been hearing about are not translating to the same number of hospitalizations as usual. But that is clearly an artifact of decreased reporting.
"Nationally (our dashboard shows) Covid-19 wastewater levels in August are about 67% of the January peak. But hospitalizations are at 19% of the January peak. It looks to us like most of that gap is due to the end of mandated hospital reporting of Covid admissions.
Why we care? Respiratory virus season is coming.
"This matters because, as I always say, most clinicians can’t really tell you to what degree a person admitted to the hospital with Covid these days is there because of that fact. Indeed, Covid “tip-overs” (infections that exacerbate chronic conditions) are the driver behind the majority of hospitalizations today. These cases count! I refer you to the example of Dr. Robert Wachter of UCSF who tipped over both literally and figuratively. Dr. Wachter shared with the world when he fell and experienced a brain bleed, requiring hospitalization. But he wouldn’t have had that fall unless he had Covid, it’s quite clear.
"As we move into our first respiratory virus season without mandated
Covid-19 reporting by hospitals, we’ll need to track these metrics and
contextualize them anew. But, that’s what we do around here."









.jpg)
No comments:
Post a Comment