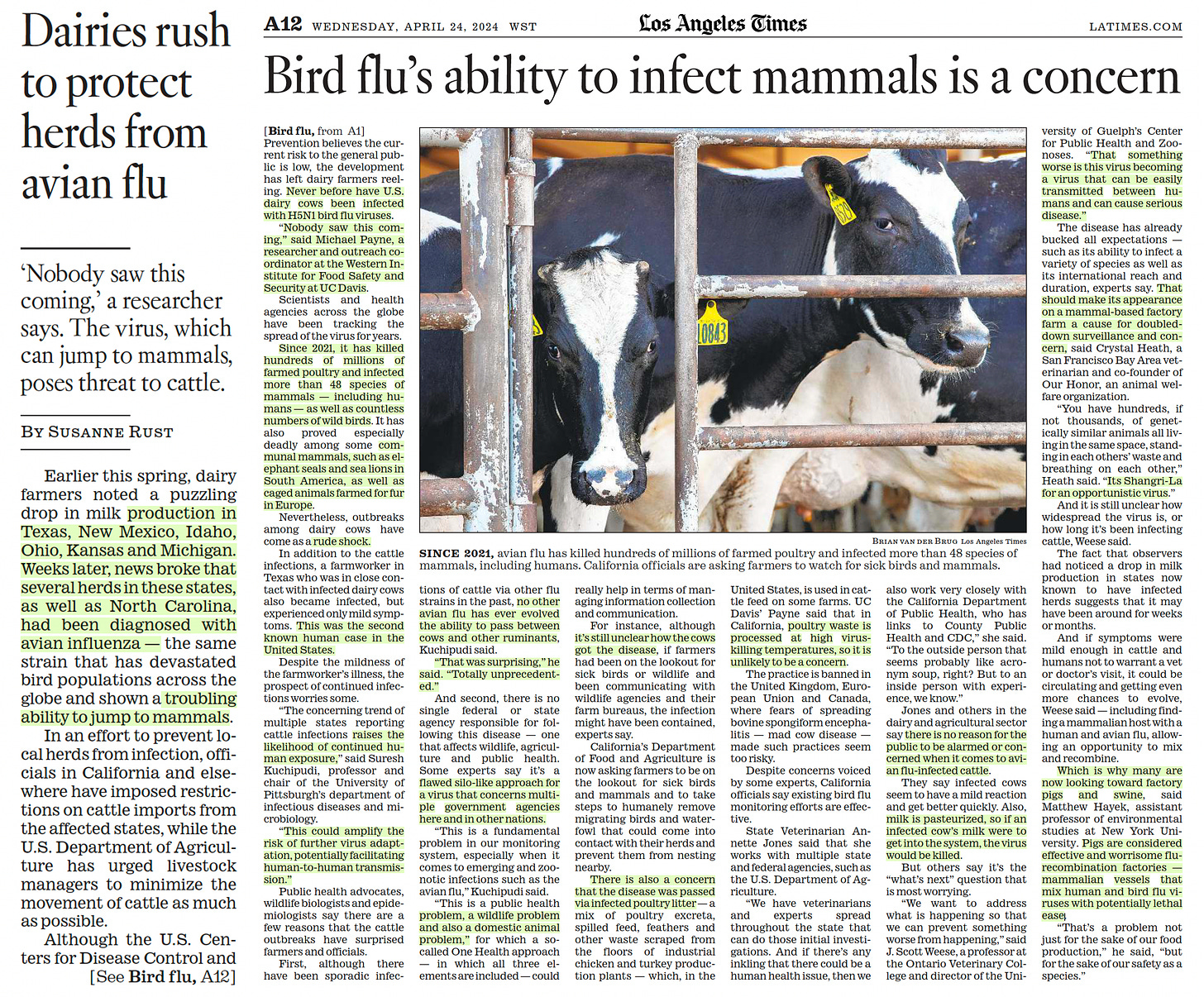
Here's another information-packed column by Julia Doubleday at The Gauntlet:
The WHO is patting itself on the back this week.
After two
years of argument and discussion, it has officially rebranded airborne
viral transmission as “through the air” transmission. Airborne particles
aren’t aerosol anymore; they’re “Infectious Respiratory Particles,” or
IRPs. Jargony language aside, the major practical implications of this
document are that, unlike previous airborne infection control guidance,
their new guidance will not, in fact, control airborne infections.
Let’s back up. To understand where we are, we have to understand how we got here.
In early 2020, the WHO had already decided COVID was not airborne. On March 28, 2020, they tweeted a famous and famously still-not-deleted fact check proclaiming this loud and clear. “FACT: #COVID19 is NOT airborne. The #coronavirus
is mainly transmitted through droplets generated when an infected
person coughs, sneezes or speaks,” the tweet reads, going on to
recommend disinfecting surfaces, staying 1m distance from others,
washing hands, and not touching your face. It’s accompanied by a graphic
that looks like it was made in 20 minutes by an unpaid intern, which
again affirms that COVID IS NOT AIRBORNE. All of the information in this
short tweet is incorrect.
It also informed the global
COVID response from top to bottom, making elimination of the virus
impossible as governments implemented an inadequate protocol for
stopping the spread.
From the beginning, the WHO was
promoting a now-disproven model of infectious disease control centered
on an artificial distinction between diseases transmitted by “droplets” -
meaning large particles emitted while coughing and sneezing which
quickly fall to the ground- and “aerosols” - meaning smaller particles
that are emitted simply by breathing that can hang in the air like
smoke. The best layman’s summary of the droplet vs. airborne scandal can
be read here, in Megan Molteni’s thorough piece “The 60-Year-Old Scientific Screwup That Helped Covid Kill”, published at Wired in May of 2021.
Molteni’s
piece follows a small group of intrepid scientists- Linsey Marr, an
aerosol expert, Lidia Morawska, an atmospheric physicist, Yuguo Li, an
indoor air researcher at the University of Hong Kong, and Katie Randall,
an infectious disease historian, as they attempt to convince the WHO
and other health institutions to take airborne spread of COVID
seriously. In the process, they dig into the deep roots of scientific
misinformation that led to the creation of the droplet vs. airborne
dichotomy; incredibly, there was never any strong
evidence to indicate that most viruses were spread via heavy “droplets”
that fall to the ground. It was quite simply a creation of convenience
predicated on poor assumptions, misinterpretations, and conflations. I
recommend reading the whole piece, but in essence, institutions have
been believing what they wanted to believe about airborne transmission
for a long time.
It should also be noted that the
institutional and financial motivations for failing to acknowledge
airborne transmission of COVID and other viruses are pretty
straightforward; it is, quite simply, far more expensive to implement
proper infection control protocol for a virus that spreads through the
air because a human is breathing than it is to implement infection
control protocol for a virus that spreads when someone sneezes on you.
This paper, titled “Coronavirus Disease 2019 and Airborne Transmission: Science Rejected, Lives Lost. Can Society Do Better?” and
co-authored by Morawska, provides an inside look at the WHO’s refusal
to contend with scientific evidence, their allergy to all discussion of
airborne transmission, and their dismissive, rude and stubborn behavior
as aerosol experts came together to try and correct their incorrect
guidance as COVID gained ground. “We alerted the World Health
Organization about the potential significance of the airborne
transmission of SARS-CoV-2 and the urgent need to control it, but our
concerns were dismissed,” affirm the authors, going on to discuss their
formation of the so-called Group 36:
On 29
March [2020], Morawska drafted a message in the form of a petition to
the WHO director general (DG) and compiled a list of experts—colleagues
of high international standing from around the world—whom she knew had
been working on airborne transmission for many years from various
angles, including aerosol physics, virology, public health, clinical
medicine, infection prevention and control, building engineering, and
facility management. She had worked on this broad topic over the years
with several of these individuals. The next day she contacted all of the
identified experts, explaining the problem, presenting the draft, and
asking if they would like to support the petition. Every one of them did
so, and some suggested names of additional experts to include. The list
expanded to 36 names, a sizable group; although we knew that many more
experts could have been enlisted given more time this was a manageable
group who represented a breadth of expertise from around the world. This
is how “Group 36” was born.
The WHO did not respond
well to this petition, which again, was signed by the foremost experts
in airborne transmission. Multiple meetings yielded nothing but
irritated dismissal on the part of WHO, with participants recalling:
We
were backed into a defensive position during the call, while we tried
to make our points. After the call was finished, disappointed and
frustrated, we wondered, Why are they acting like this? Why are they so
bluntly rejecting our arguments?
Email correspondence
between the two groups- the WHO and the aerosol expert petitions- is
attached to the paper. The correspondence shows that the WHO either
failed to grasp or represented themselves as failing to grasp the points
made by the aerosol experts. Multiple times, they repeat false claims
about how sure they are that COVID is spread via “droplets”, that
respirator-style masks only need to be worn during AGPs
(aerosol-generating procedures, an incorrect claim that is still
repeated by medical practitioners today), and that fomites are a
significant source of COVID transmission (they are not). They also
repeatedly make arguments from authority, pointing to individuals who
agree with them while refusing to engage with the science itself. In one
impressive piece of circular logic in an email dated April 11, 2020,
the WHO states:
To our knowledge and after careful
review, available evidence on SARS-CoV-2 supports that the predominant
route of human-to-human transmission of this virus is through
respiratory droplets and/or contact routes. We note that also guidance
from CDC, ECDC, and many other organizations all state that the mode of
transmission of COVID-19 is primarily respiratory droplets and contact.
In
this excerpt, the WHO cites the guidance of other organizations which
are turn following WHO guidance. They cite no studies to shore up their
claims that COVID must be spread via droplets, but sneeringly point out
that the aerosol scientists have not produced “peer reviewed” studies
demonstrating airborne spread. In April 2020, of course, it was
impossible for any peer review to have been completed concerning a virus
that was then a few months old.
Throughout the debate
between the powerful WHO players and the upstart aerosol experts, the
threshold of “proof” for airborne spread was unreachably high, while the
threshold of “proof” for droplet spread was nothing at all. WHO
continually states that they know COVID is spread via droplets while failing to address any of the actual scientific content of the petition from Group 36.
The work of these scientists, along with dozens of others, led to the groundbreaking realization that all common
respiratory viruses- colds, flus, RSV, etc- are being spread in a
manner that would have formerly fallen on the “airborne” side of the
false airborne/droplet dichotomy. Hence the need to rethink the
terminology entirely- and common infection control practices.
Once
this was established, we stood at the precipice of a new era of disease
control; imagine a clean air revolution in daycares, drastically
cutting down the now-spiking rate of childhood illness.
But three years after Molteni’s rundown was published, most medical
institutions and government bodies are still practicing and recommending
droplet infection control measures for COVID. What happened?
First,
there’s been a lack of consistent, public communication. Today, most of
the public still uses the mental model of “droplet” spread to
understand COVID transmission- and that includes doctors and
administrators in medical settings. Measures like social distancing,
handwashing, wiping surfaces, and wearing surgical masks (not respirator
style masks that form a seal) are insufficient to control the spread of
COVID-19; some of them are out-and-out pointless. While things like
surgical masks and distancing do reduce likelihood of transmission
somewhat- not entirely- fomite transmission of COVID has never been
documented and surface disinfection is wholly irrelevant to spread.
The
failure to loudly communicate that our global health organizations were
devastatingly wrong about something they stated with a high degree of
confidence is perhaps unsurprising. That their claims led to 20-30
million deaths and counting, all the more so. In order to correct all
the misinformation that the public, doctors, hospital administrators,
health bodies and public officials absorbed during the full-court press
to mitigate COVID with insufficient droplet measures, the WHO would need
to loudly and publicly repeat that all their prior guidance was wrong.
Not only that, but it was wrong because they lied;
it’s true that they seem to have really believed their own
misinformation, and in that sense, they approached the conversation
honestly. But it was a lie to say they had proof, that they knew beyond a doubt, that COVID was not airborne.
Take WHO’s new Chief Scientist Jeremy Farrar’s comments this week, for example. He states:
In
January, in February, in March, in April of 2020, the certainty of the
scientific evidence compared to six months later, a year later, now,
four years later, April 2024, is completely different.
In his defense of the WHO’s declaration that COVID was not airborne, he is here pointing out that the scientific evidence was uncertain. That’s true; it’s also why it was so irresponsible to present the claim “COVID is not airborne” with a high degree of certainty.
A responsible body would have said “we are debating this, we don’t
know, and the precautionary principle dictates that we should implement
airborne infection control until we do.” Instead, they tweeted a graphic
with a big INCORRECT stamp over the correct statement “COVID is
airborne.” Not the language of an uncertain body communicating uncertain
science.
The WHO, rather than demonstrate humility
and contrition in the face of a world-circling failure that sent us down
an infection control dead-end, continues to double down on excusing
itself. That brings us to their newest attempt to both exculpate
themselves and give governments and medical practitioners all over the
world license to continue refusing to implement airborne infection
control, endangering patients and citizens: this dry-sounding document, “Global technical consultation report on proposed terminology for pathogens that transmit through the air.”
Not
everything in the document is terrible. On the plus side, the WHO
finally invited subject matter experts like Linsey Marr to the table.
They also were correct to eliminate the false dichotomy between airborne
and droplet spread; as it turns out, viruses that spread via
respiratory particles are contained in both large droplets and smaller
aerosolized particles that can travel far beyond the arbitrary 6-feet
range of the social distancing era. But this is where the positives end.
Instead of finally acknowledging that, since all these
aerosolized viruses can spread in a manner consistent with what was
formerly called “airborne” transmission, “airborne” infection control
measures are required to control them, the WHO attempts to have its cake
and eat it too by simply reimagining what infection control is supposed
to accomplish. Instead of ensuring that patients will not be exposed to
viruses in medical settings, the WHO is now encouraging medical
practitioners to simply follow their hearts when it comes to the spread
of COVID and other viruses. Is it an airborne “vibe”? Is it more of a
“droplet” vibe? Whichever suits, take your pick!
From their paper:
There
is NO suggestion from this consultative process that to mitigate the
risk of short-range airborne transmission full ‘airborne precautions’
(as they are currently known) should be used in all settings, for all
pathogens, and by persons with any infection and disease risk levels
where this mode of transmission is known or suspected. But conversely,
some situations will require ‘airborne precautions’. This would clearly
be inappropriate within a risk-based infection prevention approach where
the balance of risks, including disease incidence, severity, individual
and population immunity and many other factors, need to be considered,
inclusive of legal, logistic, operational and financial consequences
that have global implications regarding equity and access.
This
word salad essentially means “yeah, all these viruses can spread via
airborne transmission, but since airborne precautions are annoying and
expensive, you don’t really have to do them”. It provides legal and
institutional cover for the medical bodies who are still refusing to
acknowledge airborne spread of COVID-19 and implement proper infection
control. Vague terms like “balance of risk,” “severity,” “individual and
population immunity,” all leave open an incredibly dangerous window for
continued spread of COVID in medical settings; especially as one man’s
“mild” is, quite literally, another man’s “severe”.
The
terms “severity” and “population immunity” serve as a dog whistle to let
government bodies and medical institutions know, yes, we did finally
have to acknowledge that COVID is airborne. But don’t worry,
this doesn’t mean we’re actually going to make you do airborne
infection control. If you think it’s okay for your patients to contract
COVID, it’s a-ok by us too! “Immunity” in particular is a highly-abused
term in the context of COVID; most people achieve a temporary immunity
from vaccination and/or infection, which rapidly fades. In an effort to
normalize continual reinfection, our governments began conflating this
short-term, rapidly fading protection that varies from person to person
with the lifelong protection formerly known as “immunity”, a term which
better applies to diseases like measles or chickenpox. Herd or population immunity in the context of measles means vulnerable people are never exposed to measles. Herd immunity in the context of COVID means vulnerable people are constantly exposed to COVID. It’s all very “war is peace.”
A
note on the claim that “equity” and “access” are the true motivators
behind the WHO’s poor guidance. Here, the body is attempting to argue
that, because poor countries cannot afford proper airborne infection
control, no one should have access to proper airborne infection control;
hooray, that’s equity! Aside from the patent ridiculousness of this
argument, let’s compare this with claims the WHO made four years ago
vis-a-vis the same topic, while still claiming that airborne spread
wasn’t happening.
Email from WHO Health Operations, Infection Prevention and Control Technical Team to Group 36, April 11, 2020:
The basis for the content of WHO guidance is as follows:
1)
current evidence on SARS-CoV-2 predominant modes of transmission and
lessons learned from the evidence on SARS, MERS and other respiratory
viral infections;
2) direct experience with COVID-19 patients by frontline workers, epidemiologists, virologists and other scientists;
3)
input, discussions and consensus by a large group of international
independent experts in the fields of infectious diseases, epidemiology,
public health and infection prevention and control, with special focus
on viral respiratory infection (captured through our COVID-19 global
expert network teleconferences);
4) global perspective including equity, ethical, and implementation considerations of WHO guidelines.
The
latter is important for a global organization that needs to take into
consideration capacity across health systems in different countries;
however, under no circumstances does this aspect overcome available evidence.
WHO is always reviewing available evidence and will adapt guidance
based on this evidence – as always done for all infectious hazards.
COVID-19 is no different. Would there be evidence of
significant spread of SARS-CoV-2 as an airborne pathogen outside of the
context of AGPs, WHO would immediately revise its guidance and extend
the recommendation of airborne precautions accordingly despite the known
limited capacity to apply them in all countries, in particular in low-
and middle-income countries.
Emphasis
mine. There, in black and white, the WHO contradicts its new guidance,
stating in no uncertain terms that if COVID were airborne (it is),
airborne infection control measures should be and would be recommended, even given the difficulties and expense of instituting such protocols.
Proper infection control guidance should do one basic thing: ensure that infections are controlled.
Ensure that patients are not needlessly exposed to viruses- of any
kind- while seeking medical care. The revolutionary progress we’ve made
in understanding the behavior of viruses over the past several years,
coupled with the fantastic technology that already exists to clean the air, would mean a much healthier society if that progress were applied practically. Instead, we’re becoming a much sicker society as the WHO sinks further into denial.
This
document exists to handhold a small group of elite scientists who were
incredibly, undeniably, dangerously wrong, and allow them to continue
pushing their failed model of “infection control” which does not, in
fact, control infections. It exists to assuage their damaged and bruised
egos while assuring them they weren’t wrong to tell people to stand six
feet apart and wipe down surfaces and cover their sneezes; this is,
after all, the most practical and feasible form of infection control to
implement even if it turns out the virus itself maybe, kind of, sort of,
spreads in a completely different way.
The damage of the
WHO’s false claims continue to reverberate today. Doctors and hospitals
continue to infect their patients with flu, RSV, strep, and now COVID as
infection control measures like HEPA filtration go completely
unmentioned in the new guidance document. Hospitals continue to place
highly infectious patients close to COVID-negative patients, falsely
believing that curtains and a few feet of distance will protect
vulnerable sick people. Doctors and nurses continue to lack proper PPE,
while acquiring Long COVID at high rates and dealing with out-of-control hospital crowded all over the world.
And perhaps most damaging at all, the public has been lulled into a
sense of complacency and encouraged to believe that COVID simply cannot
be controlled. Unaware that the protocols implemented in 2020 were
plainly incorrect for mitigation and elimination, the defeatist refrain
rings out everywhere, “COVID is here to stay, there’s nothing we can
do.”
The WHO has a responsibility to engage seriously
with the science of airborne infection control and make recommendations
that minimize the spread airborne disease- not recommendations that seek
instead to minimize its own embarrassment and responsibility.

















.jpg)