"Wastewater levels are “LOW” across the US and hospitalizations, emergency department visits and deaths from COVID have decreased even more. JN.1 and its descendants are responsible for almost all COVID cases now. In the Bay Area, Santa Clara county is in the “MEDIUM” level for SARS-CoV-2 in wastewater. Stanford had a huge spike of wastewater virus a few days ago that has now resolved. There are also HIGH viral wastewater levels of SARS-CoV-2 in Mill Valley, and MEDIUM levels in Sausalito and San Rafael. Although numbers are low nationally, I personally know four people who have had a COVID infection in the last week. According to JP Weiland, about 1 in every 164 people is currently infected and there are about 200,000 new COVID cases per day across the United States. You can see wastewater levels for your county by searching on Wastewater SCAN.
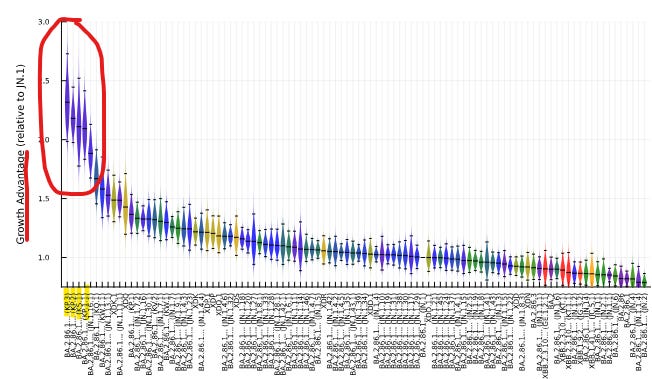
"Although we are at low virus levels for the U.S. now, variant hunters on Twitter have alerted that new JN.1 descendants with the FLiRT mutation (subvariants KP.3, KP.2, KS.1, KP.1.1) have a significant growth advantage over JN.1 and therefore may cause another COVID wave(let) in the next 6 weeks. According to Eric Topol MD and JP Weiland, JN.1 + FLiRT subvariants will probably not cause a very large wave, since our collective immune systems have seen the FLiRT mutation in past variants and since the JN.1 wave just recently happened. The latest COVID vaccine (against XBB.1.5) does provide protection against JN.1 for hospitalization and death for at least several months. We do not know yet if this vaccine will work against JN.1 + FLiRT subvariants yet, but the feeling is that the XBB.1.5 vaccine should offer at least some protection. Seniors and immunocompromised people should get their second dose of the XBB.1.5 vaccine soon.
Figure: Ben Murrell shows the growth advantage of JN.1 + FLiRT subvariants (KP.3, KP.2, KS.1, KP.1.1)
Acute COVID infections, General COVID info
"An eye-opening article came out showing that airborne SARS-CoV-2 virus can linger in a room and can infect others almost 5 hours after an infected person leaves a room. The authors used whole genome sequencing (WGS) and discovered that "genetically identical SARS-CoV-2 infected two patients who were admitted to a hospital room 1 hour, 43 minutes and 4 hours, 45 minutes after discharge of an asymptomatic infected patient".
"Remdesivir made some news. Patients who did not require oxygen on admission to the hospital, but were treated with Remdesivir were found to have 25% reduction in in-hospital mortality compared to non-remdesivir treatment at 14 days and a 17% decrease in in-hospital mortality compared to non-remdesivir treatment at 28 days. The reduction in in-hospital mortality from giving Remdesivir at hospital admission was seen with all COVID variants.
"The microbiome refers to the community of microorganisms (such as fungi, bacteria and viruses) that normally live in different parts of our bodies such as in the gastrointestinal system or the skin. A new study of the saliva of people with an acute COVID infection showed that the “oral microbiome and salivary cytokines may be predictive of COVID-19 status and severity.”
"The SARS-2 virus can infect both exocrine and endocrine cells in the pancreas. A new study shows that COVID infection can cause increased insulin resistance, and even a loss of beta cells that make insulin. The loss of beta cells was associated with lower insulin production with islet amyloidosis and necrosis. Fortunately, vaccination against COVID was shown to help with glucose homeostasis by activating insulin receptor α and insulin receptor β. The authors noted "Overall, the cumulative risk of diabetes post-COVID-19 is closely tied to age, suggesting more attention should be paid to blood sugar management in elderly COVID-19 patients."
"There were two other studies this week on age-dependent responses to SARS-2 infection. Older adults can be more susceptible to severe COVID infections. Using mass cytometry, serum proteomics, antibody assays, and transcriptional analysis, a group found that older age was associated with increased viral load, reduced ability to clear the virus, and dysregulation of immune signaling. Older adults also had higher expression of pro-inflammatory genes and proteins with severe COVID infections. In addition, herpes simplex virus and cytomegalovirus (CMV) were reactivated in the upper airways of older adults.
"Another group looked at age-specific responses to SARS-CoV-2 infection in the nasal epithelial lining and found differences in the types of cells found in the nose. In children (<12 years old), a distinct goblet inflammatory cell was seen in the cells lining their noses, along with high interferon levels which stopped viral replication. In older adults (>70 years), nasal epithelial cells infected with SARS-2 showed an increase in basaloid-like cells, which helped the virus spread. Differing amounts of ACE2 and TMPRSS2 receptors were found in nasal epithelial cells in different age groups.
From: https://www.nature.com/articles/s41564-024-01658-1
Vaccines and antiviral medications
"A modeling study of hybrid immunity from infection and from vaccination showed that the immunity wall from prior COVID infection does not last very long if people are not also vaccinated. Without vaccination, people can become reinfected with the same variant a few months after their first infection. Higher vaccination levels in a community provided a better immunity wall to stop secondary reinfections with the same variant.
"Newer mutations help the SARS-2 virus to escape from some monoclonal antibodies that worked against prior variants. A group isolated 28 potent monoclonal antibodies and found that some of them regained the ability to neutralize newer variant BA.2.86. JN.1 is a descendant variant of BA.2.86.
"A new study from Yale shows that neosporin ointment placed in the nose may help prevent COVID and the flu. Intranasal generic antibiotic neomycin increased interferon expression in the nose and protected mice and hamsters from COVID infection and from Influenza A. In humans, Neosporin was also found to increase antiviral interferon expression in the nose.
Long COVID
"On April 15, Dr. Jeremy Faust interviewed NIH Director Monica Bertagnolli MD. During their conversation, Dr. Bertagnolli said that data shows that live SARS-CoV-2 virus can persist in tissues for months or even years. She also discussed the need for better antiviral medications to stop viral reservoirs in the body to possibly prevent Long COVID. This was the first time that someone from the government said that there are definitely viral reservoirs of SARS-CoV-2 in the body.
"From their interview:
“Faust: I just want to follow up on something you said a moment ago about where this virus can be found in tissues. Are you suggesting that Long COVID is actually, the mechanism of that persistent live virus in humans?
Bertagnolli: We see evidence of persistent live virus in humans in various tissue reservoirs, including surrounding nerves, the brain, the GI [gastrointestinal] tract, to the lung.
Faust: OK. And you're saying this goes beyond the PCR's [polymerase chain reaction test] ability to get it in a regular swab so that we are missing chronic cases of SARS‑CoV‑2?
Bertagnolli: Correct. The virus can persist in tissues for months, perhaps even years.
Faust: OK. I think that's certainly one theory, but I'm not sure that that's settled. Is that fair? I mean, there's one thing between people who are autopsy, they died of viral sepsis, as opposed to people walking around. Is there a distinction there?
Bertagnolli: Our emerging data shows that the virus can persist into tissues in the long term, and I think that's really critical because it does help us think about possible ways to combat it, one being better antivirals. I think there's a lot of focus on developing new antivirals as a possible way of preventing long COVID, and the other might be more aggressive treatment with antiviral therapy upon initial diagnosis.”
"This week, a study in Nature magazine stated that many people with Long COVID have resolution of immune dysregulation at 24 months. But, this study had many flaws. The authors’ definition of Long COVID was if someone had “fatigue, dyspnea or chest pain.” They did not study people with cognitive dysfunction, orthostatic intolerance, sleep disturbances or post-exertional malaise. More than 20% of their Long COVID patients were lost to follow-up. In addition, some people with Long COVID in the study were reinfected within the 24 months. While they said that immune dysregulation had resolved by 24 months, their data showed that people with Long COVID still had significant EBV T-cell exhaustion at 24 months. There are a lot of problems with this study and I anticipate that it will be retracted or changed.
"Congratulations to Professor Akiko Iwasaki of Yale who was named one of TIME magazine’s 100 most influential people! Dr. Iwasaki studies how the immune system fights off viruses at mucosal surfaces. More recently, she has been investigating the pathophysiology of Long COVID and has been working on a mucosal vaccine against SARS-CoV-2.
ME/CFS and Long COVID
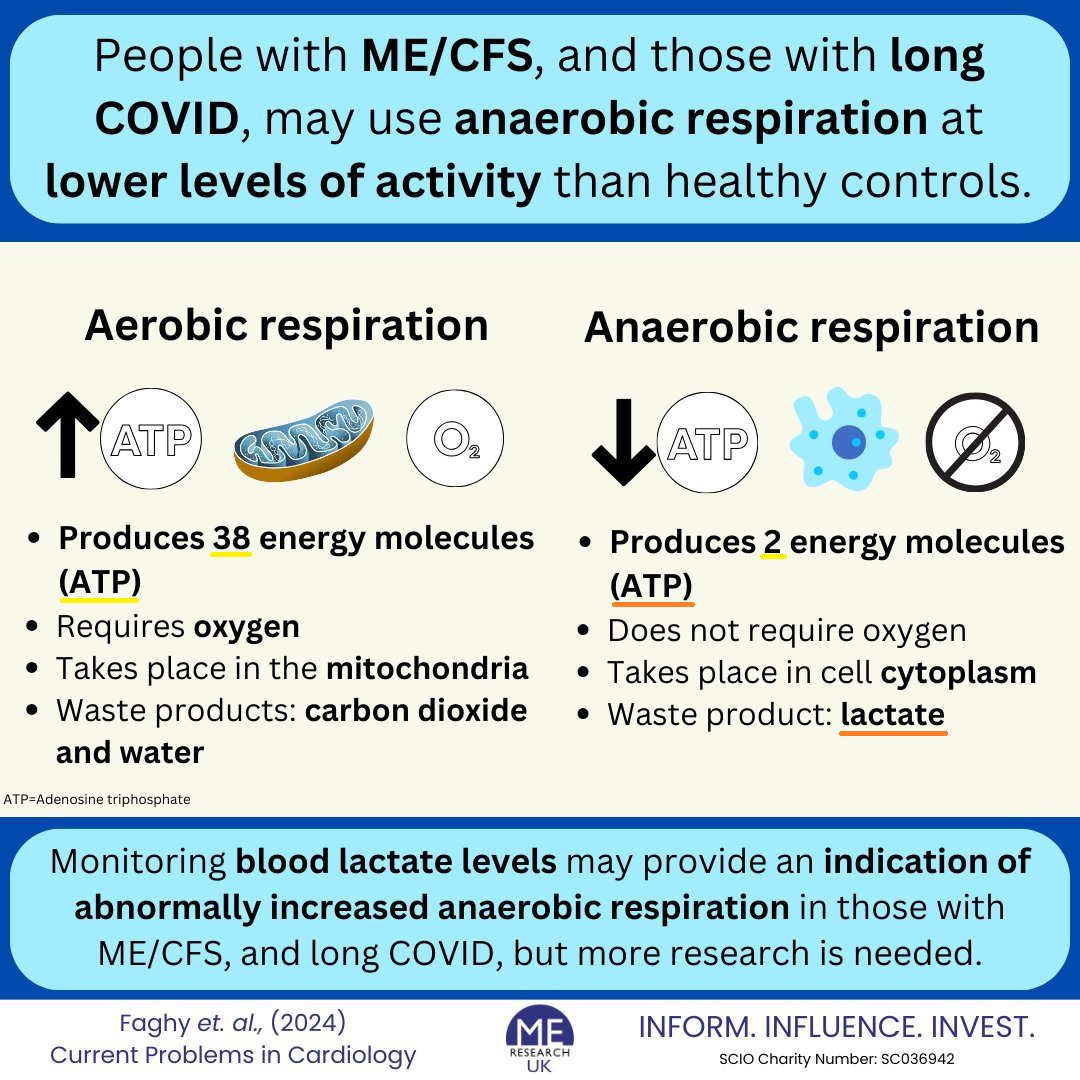
"Elite athletes test their lactate levels to see if they have pushed their bodies into anaerobic respiration. A group from the UK suggests that lactate monitoring could also be used in people with ME/CFS and with Long COVID to see when they switch to anaerobic respiration to produce energy. Aerobic respiration takes place in the mitochondria and is very efficient at producing 38 ATP molecules from oxygen. In contrast, anaerobic respiration is not efficient- it only makes 2 ATP energy molecules and produces lactate as a waste product. People with Long COVID are not able to extract oxygen in their muscles and tissues like healthy people can, and therefore, they rely on anaerobic metabolism more often. Anaerobic metabolism in people with ME/CFS and Long COVID is thought to be one reason why they get post-exertional malaise from minimal movement or exercise. As ME Research UK stated, “monitoring blood lactate levels may provide an indication of abnormally increased anaerobic respiration in those with ME/CFS and Long COVID, but more research is needed.”
From: https://twitter.com/MEResearchUK/status/1779872308452065313
"A new NIH initiative is trying to find out if Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) are the same disorder. Authors in Neurology Today reviewed an excellent article from Feb 21, 2024 from the NIH on post-infectious myalgic encephalomyelitis/ chronic fatigue syndrome (PI-ME/CFS). Dr. Avindra Nath stated “We believe these [ME/CFS and Long COVID] are virtually the same disease, … and they should be managed and studied in multidisciplinary clinics focused on post-infectious syndromes.”
"Below is the summary slide from the February article which shows COVID infection causes abnormal changes in the microbiome of the gut. This, in combination with immune dysfunction, leads to decreased metabolites that are used to make neurotransmitters in the brain. The lower levels of tryptophan and other metabolites causes several things to happen in the brain which then affect the heart and the skeletal muscles.
The catecholamine nuclei in the brain release less catechols, which affects the autonomic nervous system causing increased sympathetic function and decreased parasympathetic activity leading to decreased heart rate variability.
Abnormalities in the Hypothalamus decrease activation of the right temporoparietal junction which affects motor cortex function and leads to decreased motor strength.
"Together, autonomic dysfunction of the heart and central motor dysfunction via the brain leads to decreased muscle strength which is seen as a decrease in physical activity and ability.
















.jpg)
No comments:
Post a Comment