It is important to compare the CDC NWSS wastewater COVID data and WastewaterSCAN data, as each has gaps. The CDC’s NWSS data, last reported on November 30, 2024, shows LOW nationwide levels of COVID in wastewater. Meanwhile, WastewaterSCAN, updated on December 4, reports MEDIUM levels of SARS-CoV-2 across the U.S. However, WastewaterSCAN excludes data from 12 states, including New Mexico and Arizona, which have very high COVID levels in wastewater.
The CDC covers more states but updates less frequently, while WastewaterSCAN provides more current data. Sara Anne Willette's composite SARS-CoV-2 wastewater map integrates both sources and, as of December 3, shows VERY HIGH levels in Nebraska and HIGH levels in Arizona, New Mexico, South Dakota, Alabama, and Massachusetts.
JP Weiland predicts a more mild winter COVID wave in Europe and North America because there are no new variants on the horizon yet that are threatening. He likens last year’s variants which caused the winter (JN.1) wave and the summer (FLiRT/FLuQE) wave to a race car with lots of power and the present XEC variant as a children’s bicycle in comparison. That’s not to say that there won’t be a winter 2024 COVID wave, but he anticipates that there will be significantly fewer COVID cases this year than last year. As of December 2, JP Weiland states that there are 196,000 new COVID infections per day in America now and that about 1 in every 170 people is currently infected.
Variants
As of December 7, the XEC variant represents 44% of COVID cases now and KP.3.1.1 has decreased to 39% of cases. There are no other concerning variants being watched at this time. XEC has been increasing more slowly than other variants have in the past.
Acute COVID infections, General COVID info
A new study from UCLA shows that SARS-CoV-2 can infect retinal pigment epithelial (RPE) cells in the eye which may lead to retinal damage and blindness over time. The type of inflammation that the COVID virus causes in mice and in vitro causes changes that are similar to age-related macular degeneration (AMD), a major cause of human blindness. Increased AMD risks are seen in other viral infections like HIV, but the risks of AMD blindness are on a much larger scale with COVID since so many people have been, and continue to be, infected with SARS-CoV-2.
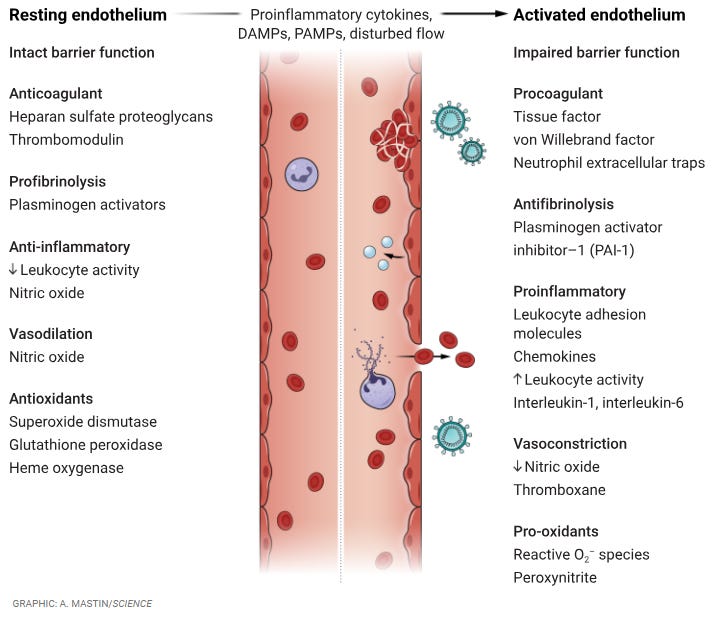
Endothelial cells line blood vessels and play a key role in regulating blood flow and preventing clotting. In COVID, the SARS-CoV-2 virus triggers inflammation that disrupts these functions, leading to blood clots in arterial and venous microvessels, inflammation, organ damage and ischemic stroke. Impaired blood flow and fibrosis can persist long after infection, highlighting the need for careful management of inflammation and clotting in acute COVID infection and long after the acute infection has resolved. This article in Science reviews the mechanisms of endothelial function in health and disease.
From: https://www.science.org/doi/10.1126/science.add2962
Pediatrics
The CLoCk study followed 12,632 preteens and teens aged 11–17 in England for 2 years and found that 7.2% of them had Long COVID at 3, 6, 12 and 24 months after acute COVID infection. The most common Long COVID symptoms reported were fatigue, trouble sleeping, and headaches. Those who were reinfected with COVID had more symptoms than those with one prior COVID infection. The findings emphasize the need for longitudinal studies in children and young people ages 11 to 17.
Neutrophilic granulocytes are a type of white blood cell that helps fight infection. A study from Hungary of 129 children with Long COVID found that decreased neutrophil function, as seen by lower superoxide production in neutrophils, correlated with worse Long COVID symptoms in children. The children with abnormal neutrophils had severe fatigue and poorer quality of life.
Pregnancy
A very small study from Augsburg, Germany shows that there are sex-differences in immune responses in the placentas of pregnancies complicated by maternal COVID infection. The placentas of male infants showed increased CD163-positive macrophages and in PD-L1 in the decidua, both in acute infections and in post-acute COVID. This was not seen in placentas of female infants. In general, higher levels of PD-L1 makes T cells more immune tolerant. Further research is needed to understand the long-term implications of these immune changes on offspring health.
Long COVID
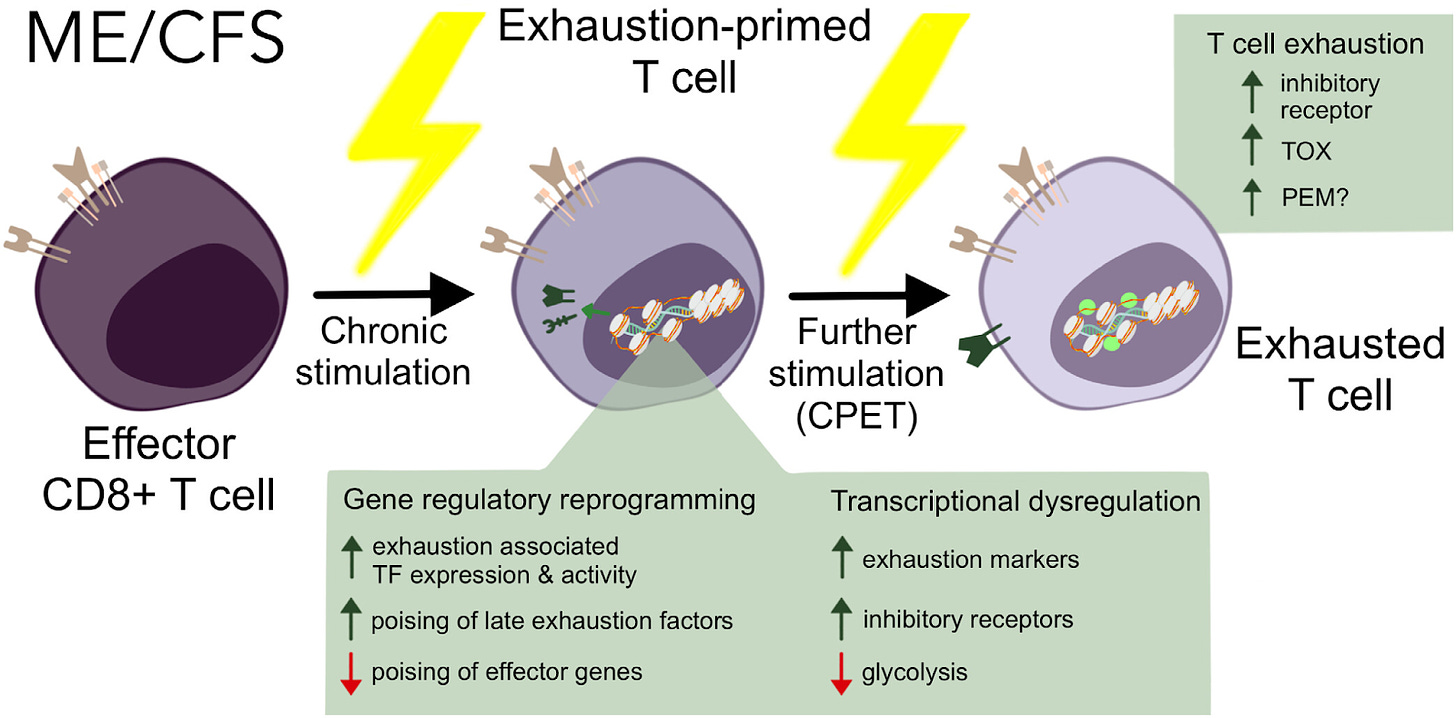
An important new study from Cornell looked at how the immune system is affected in people with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) using transcriptional and epigenetic analysis. They found that CD8+ T cells show markers of exhaustion including altered gene expression, metabolic reprogramming, and reduced immune response capabilities which make them less able to fight infections. The evidence shows that ongoing stimulation of T cells by a chronic viral infection or another inflammatory process in ME/CFS causes them to become exhausted and unable to do their job effectively. This is relevant to Long COVID since 60 to 70% of people with Long COVID also have ME/CFS and the information on T cell exhaustion may help in the development of new treatments for both diseases.
Fig. 5. Model of proposed ME T cell mechanism of action via exhaustion.
From: https://www.pnas.org/doi/epub/10.1073/pnas.2415119121
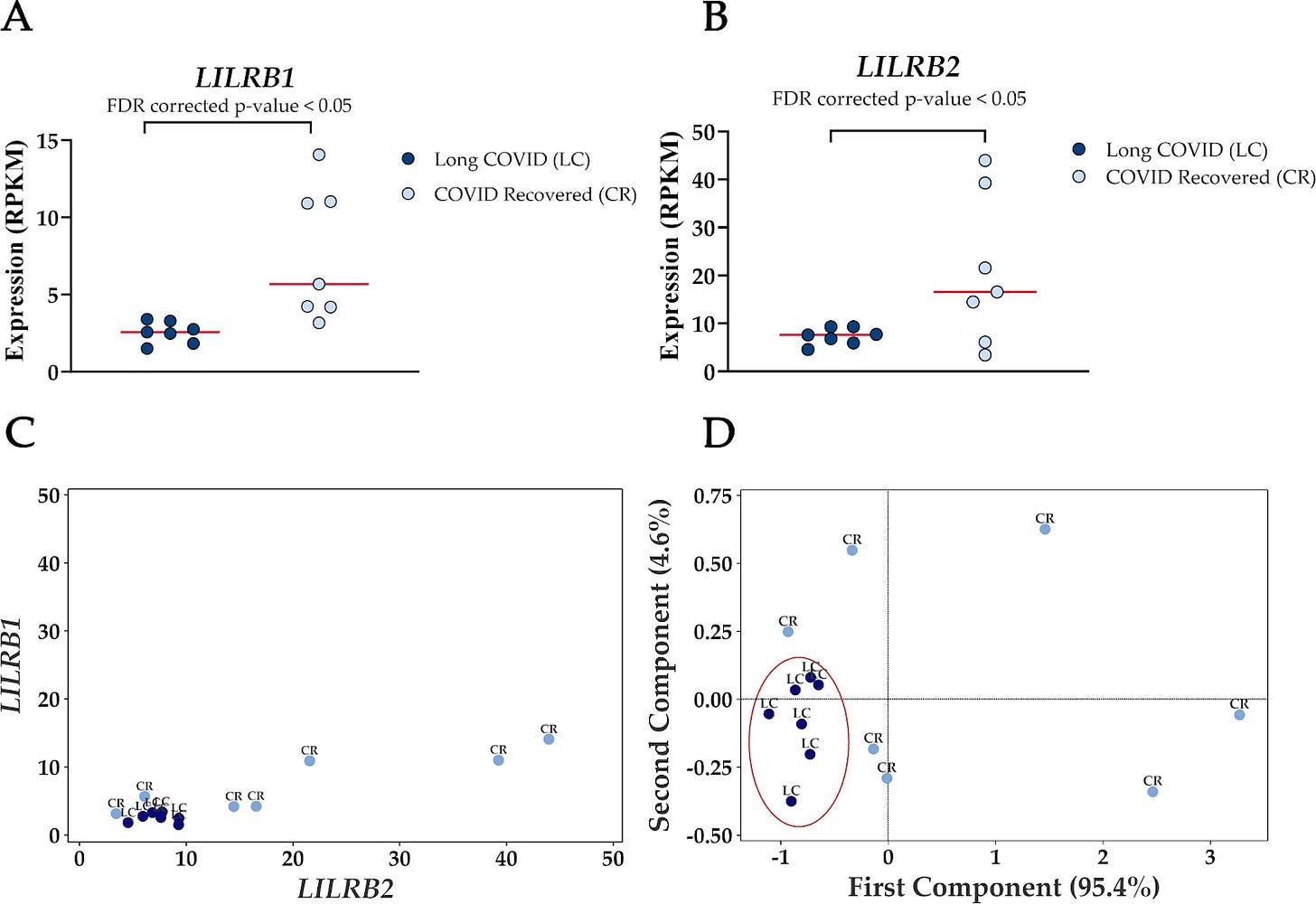
In a pilot study six months after COVID infection, the transcriptomes of peripheral blood mononuclear cells (PBMCs) were evaluated by RNA-Seq in 7 people with Long COVID and 7 recovered controls. Seventy genes were either up or downregulated. A pro-inflammatory state in Long COVID PBMCs as compared with COVID-recovered PBMCs was noted. Leukocyte immunoglobulin-like receptors LILRB1 and LILRB2 genes were downregulated in PBMCs of people with Long COVID and the mRNAs of these genes could discriminate between the small cohort of people with Long COVID from the COVID recovered blood samples with 100% accuracy. Larger studies are needed to confirm these results, but LILRB1 and LILRB2 levels in PBMCs may potentially be a biomarker for Long COVID.
Figure 5. Reduced expression levels of LILRB1 and LILRB2 in blood-derived PBMCs effectively differentiate Long COVID patients from COVID recovered individuals.
From: https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1450853/full
Long COVID and the Brain
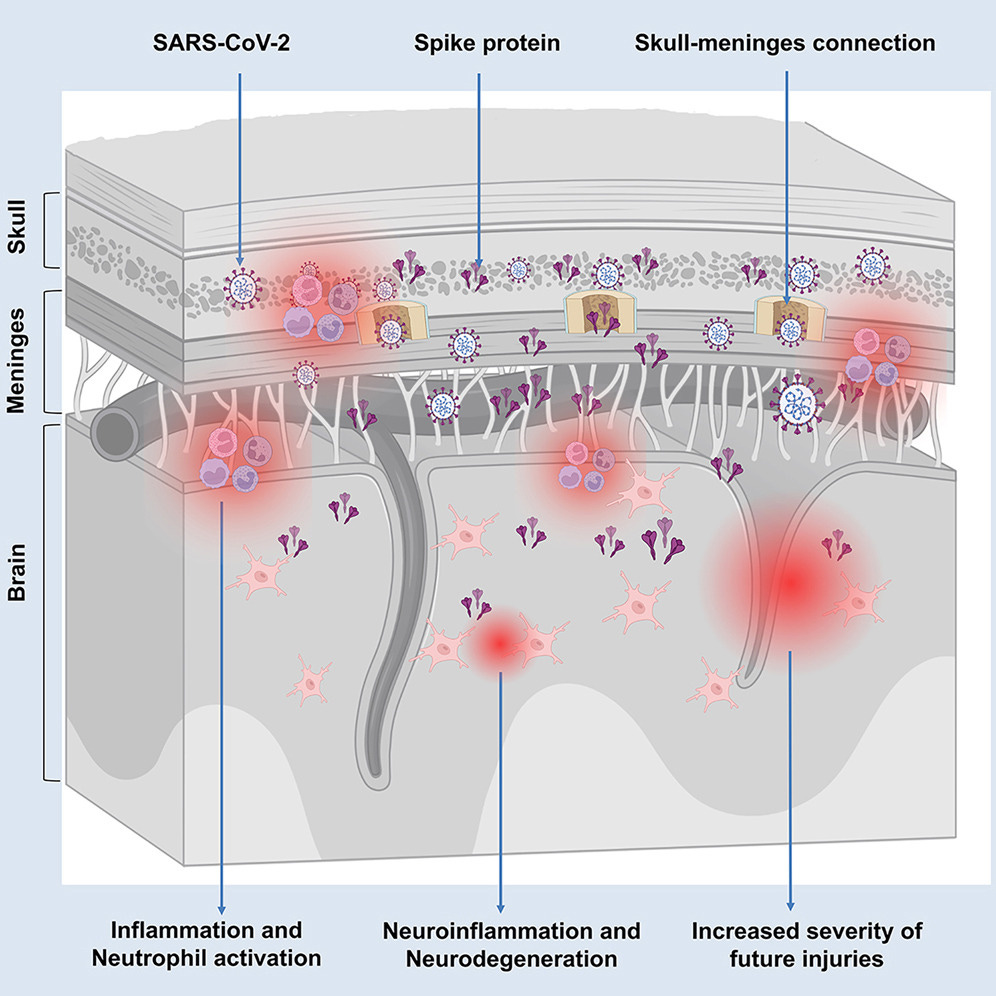
SARS-CoV-2 infection can have lingering effects on the brain according to an intriguing new paper with must see videos from Ali Ertürk’s lab. His lab uses a special technique utilizing AI that allows views down to the cellular level in tissues. In people who had a COVID infection in the past, 60% were found to have an accumulation of SARS-CoV-2 spike protein in their skull bone marrow or meninges surrounding the brain on post-mortem exam up to 4 years after COVID infection. Living Long COVID patients were found to have elevated neurodegeneration biomarkers in their cerebrospinal fluid (CSF) including significantly elevated Tau, neurofilament light chain (NfL) and glial fibrillary acidic protein (GFAP). The chronic brain inflammation from persistent SARS-2 spike protein may be causing cognitive dysfunction in people with Long COVID, as well as increased risk of strokes and brain injury. In mice, injection of the SARS-2 spike protein alone induced neuroinflammation and caused anxiety-like behavior. Vaccination with mRNA vaccines was found to reduce the level of spike protein in the skull by 50%. The authors note that “removal or inhibition of spike proteins may become an important way of treating the sequelae of COVID-19.”
From: https://www.sciencedirect.com/science/article/pii/S1931312824004384?via%3Dihub
Scientists from the University of Montreal found that a small peptide called P3 in the SARS-CoV-2 spike protein acts like bacterial superantigens Staphylococcal Enterotoxin B (SEB) and Staphylococcal Enterotoxin H (SEH). “Like SEB and SEH peptides, P3 stimulated 25-40% of human CD4+ and CD8+ T cells, increasing IFN-γ and granzyme B production.” Giving the P3 peptide to mice led to upregulation of proinflammatory cytokines IL-1β, IL-6, and TNF-α.
Could the P3 portion of the persistent SARS-CoV-2 spike protein found in the skull bone marrow and the meninges in the Ali Ertürk study above be causing the neuroinflammation and neurodegeneration in the brains of people who previously had a COVID infection? It would be interesting to study this further.
This week in his blog, Dr. Ryan McCormick discussed an interesting review of Long COVID by Dr. Daniel Griffin of “This Week in Virology (TWIV)” and “Parasites Without Borders” that I hadn’t previously seen. Dr. Griffin’s article reviews physiological and biochemical mechanisms driving Long COVID including immune dysfunction, mitochondrial issues, and lingering viral remnants. Evidence-based therapeutic options, including vaccination, probiotics, antihistamines, and cautious exercise, were discussed in this Long COVID review as well.
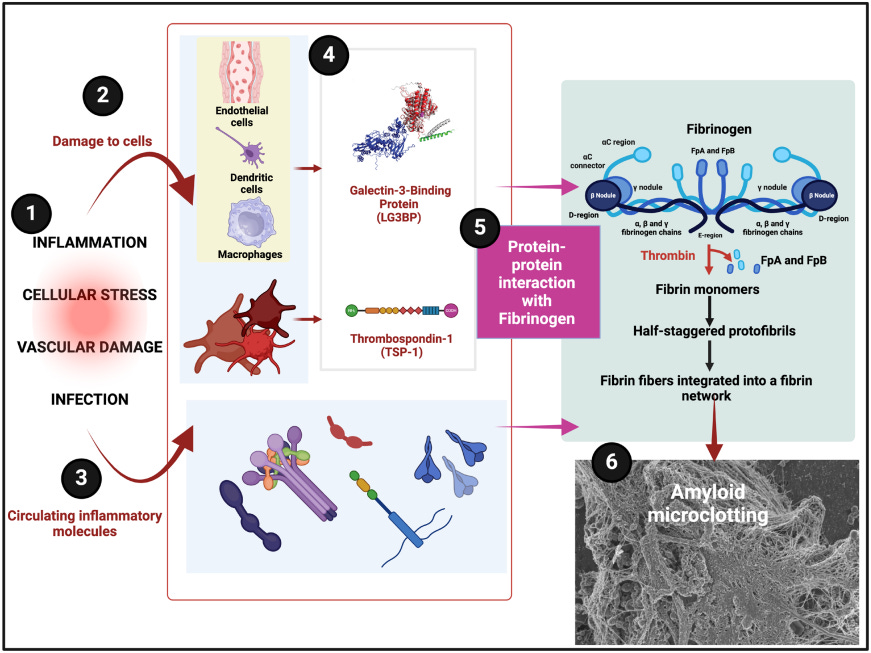
Drs. Kell and Pretorius analyzed proteins in blood clots associated with different diseases. They found abnormal amyloid clots in Long COVID, also referred to as fibrinaloid microclots, that are notably difficult to break down. "Galectin-3-binding protein and thrombospondin-1 seem to be especially widely associated with amyloid-type clots, and the latter has indeed been shown to be incorporated into growing fibrin fibres.” The authors postulate that these two proteins may be useful as biomarkers for diseases such as Long COVID that make amyloid from the polymerisation of fibrin(ogen) into an amyloid.
Figure 4: Illustration of the pathways from inflammation-induced cellular damage to the formation of amyloid microclots, highlighting the roles of two notably amyloidogenic proteins (LG3BP and TSP-1) in abnormal fibrinogen interactions and the resulting fibrinolysis-resistant clot structures.
From: https://www.biorxiv.org/content/10.1101/2024.11.29.626062v1.full.pdf
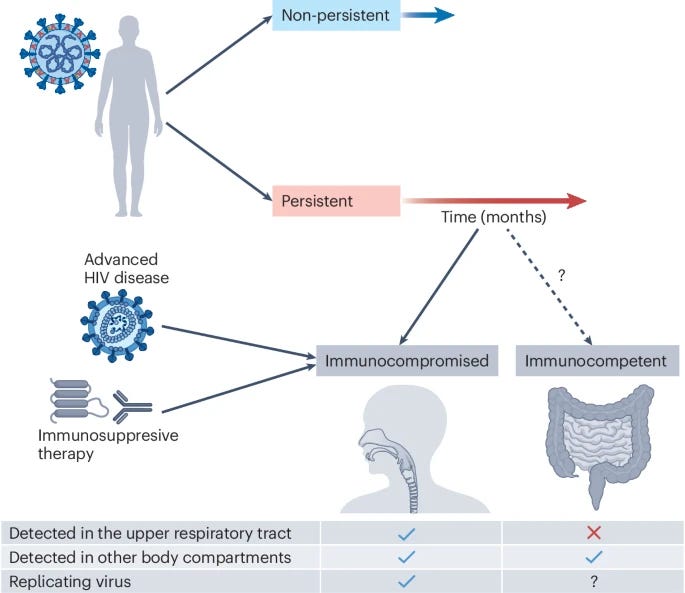
Another review looked at viral persistence in two different groups- persistent SARS-CoV-2 infections in immunocompromised people versus persistent virus or parts of the SARS-CoV-2 virus in people with Long COVID. They discussed “SARS-CoV-2 persistence mechanisms, the approximate frequencies of persistent infections, accelerated evolution in persistent infections and why persistent infections may form variants of concern and account for hot spots of variant emergence. We [They] also briefly cover the symptoms and management of persistent infections, and the connection between persistent infections and post-COVID conditions.”
From: https://www.nature.com/articles/s41579-024-01125-y
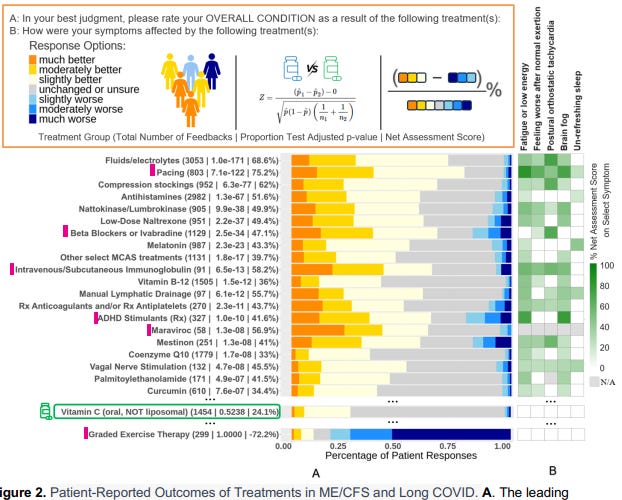
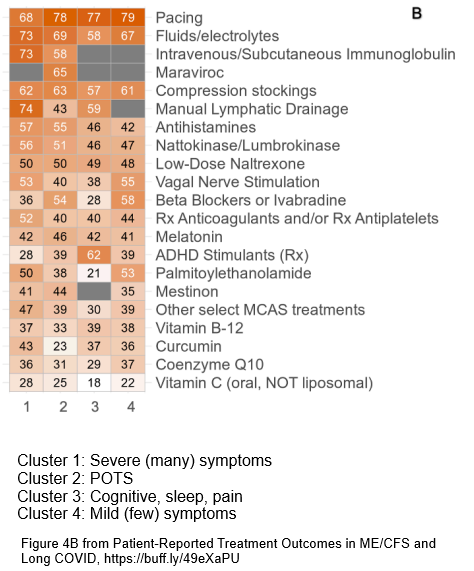
Pharmacist Dr. Martha Eckey surveyed 2125 people with ME/CFS and 1800 people with Long COVID to see what treatments had helped them or not. She then worked with scientists from Harvard and Stanford using AI to identify 4 clusters of ME/CFS and Long COVID patients that were most helped by different treatments. The supplemental materials in this paper show the numbers of people who responded for each of the treatments, as some treatments were used less commonly. The treatments that helped the most are shown below in the two figures.
Figure 2
From: https://www.medrxiv.org/content/10.1101/2024.11.27.24317656v1.full.pdf
Figure 4B: Patients Subgroups with Distinct Symptom Profiles and Treatment Efficacies
From: https://www.medrxiv.org/content/10.1101/2024.11.27.24317656v1.full.pdf
The Visible Health wearable measures heart rate variability (HRV) and is used by people with complex chronic illnesses like ME/CFS and Long COVID to understand their energy envelope. A new preprint surveyed 1,301 users of the Visible mobile app with self-identified ME/CFS or Long COVID and showed that 77% had symptom improvements, 85% felt more in control of their condition, and 94% gained a better understanding of their energy budget. In this study, pacing with the use of home-monitoring of HRV appears to be helpful for people with energy-limiting chronic illnesses.
Svetlana Blitshteyn et al. discuss in their new paper that Postural Orthostatic Tachycardia Syndrome (POTS) and other common autonomic disorders are different from functional neurologic disorders (FND) and have established diagnostic criteria, including measurable changes in heart rate, blood pressure, and cerebral perfusion during tests including the tilt table test. Misdiagnosing autonomic disorders as FND can lead to inappropriate treatments and delays in care. It is important to accurately diagnose POTS and other autonomic disorders so that the appropriate treatment can be started.
H5N1
H5N1 bird flu has been found in North America since 2021 and recently has been spreading to dairy cattle, wild birds and poultry. There have been some (50+) cases of avian flu in people who work with infected cattle or poultry, but cases so far in humans have mostly been mild with the exception of the teenager in Canada who was critically ill with H5N1. Historically, H5N1 avian flu has had up to a 30% fatality in humans.
Researchers analyzed what genetic changes would allow this H5N1 virus to fully adapt to be able to infect humans easily and it turns out that only one mutation would be needed- a single mutation of Q226L in the hemagglutinin (H) protein. Since there is now a huge reservoir of dairy cattle infected with H5N1 in California, there is concern that if the Q226L mutation happens, there could be a significant risk for an H5N1 pandemic in humans. Therefore, we really need to get the large outbreaks in animals under control and we need to follow changes in the virus closely.
As of December 6th, the USDA is finally requiring bulk testing of raw milk for the H5N1 bird flu virus. Recently, there has been an increase in dairy cattle herds with H5N1 as well as poultry flocks in several states including California. "The latest outbreaks push California’s total since the virus first turned up in Central Valley dairy cows in late August to 506 [herds]. The national total is now 720 [dairy herds] from 15 states." The USDA is not counting cattle herds who become reinfected with H5N1, even though they are contagious.
Sara Anne Willette is now posting the latest data on H5N1 avian flu infections in cattle, pigs, poultry, wild mammals, and wild birds here.
Other news:
Toxic epidermal necrolysis (TEN) and Stevens–Johnson syndrome (SJS) are severe cutaneous drug reactions that can be fatal and for which there was no cure. Using single-cell, deep visual proteomic testing, researchers discovered that the JAK/STAT and interferon signaling pathways were drivers of TEN and SJS and that targeted JAK inhibitor medications could cure these awful diseases.
A new monoclonal antibody against interleukin-5 receptor-α called benralizumab (ABRA) was found to be able to treat asthma and COPD.
The Human Cell Atlas is being made by more than 3,600 scientists from over 100 countries and has analyzed more than 100 million cells from 10,000+ people, revealing thousands of cell types, including previously unknown ones like ionocytes, which may help treat diseases like cystic fibrosis. Advances in single-cell sequencing and AI have enabled breakthroughs, such as understanding how cells evolve, mapping biological systems like the gut and brain, and linking genes to diseases and potential therapies. The first full draft of this groundbreaking project, expected by 2026, is transforming our understanding of health and disease. New research from the Human Cell Atlas Consortium was reported last week.
From CNN: “The milestones made public Wednesday include mapping all the cells of the gut; producing a blueprint of how human skeletons form in utero; understanding the basic structure of the thymus, an organ that plays a key role in how the immune system functions; mapping the molecular architecture of the placenta; and building an atlas of human vascular cells.”
A different atlas, The "Atlas of the Plasma Proteome in Health and Disease", is a large-scale study that analyzed plasma proteins in over 53,000 adults from the UK Biobank, linking 2,920 proteins to hundreds of diseases and traits. This research identified thousands of protein-disease associations and highlighted potential biomarkers for diagnosis and treatment. The findings also include insights into protein roles in precision medicine, sex differences in the plasma proteome, drug repurposing, and disease prediction, all of which are made publicly accessible to support further research in health and disease management.
Anthem Blue Cross Blue Shield announced that they would “no longer pay for anesthesia care if the surgery or procedure goes beyond an arbitrary time limit." Satirist Dr. Glaucomflecken (Dr. Will Flanary) posted this video on December 5th and by the next day, Anthem Blue Cross Blue Shield reversed their crazy policy.
The thymus is a gland in the chest that helps T cells (Thymus cell lymphocytes) to mature so that they can react to foreign invaders like infections or cancer in the body. Starting in adolescence, as people age, their thymus shrinks and produces fewer T cells which reduces the immune system's response to vaccines, infections, and cancer. A new study shows that reduced RANK-RANKL (Receptor Activator of Nuclear Factor κB (RANK)–RANK ligand (RANKL)) signaling contributes to the decline in thymus function in aging mice. Giving RANKL to older mice restored the structure of the thymus and boosted immune responses to vaccines and tumors. This research suggests that targeting the RANK-RANKL pathway could help combat immune aging and improve thymic health.
Two new studies (here and here) show that RSV monoclonal antibody drug nirsevimab (Beyfortus) provides excellent protection to infants and young children against RSV.
Dick Van Dyke will turn 99 years old next Friday. Van Dyke is featured in a new music video with Chris Martin of ColdPlay for their latest song “All My Love” that showcases Van Dyke’s family and his long career.
Atlantic Records
Notre Dame in Paris reopened today with a morning and evening mass.
Here is a photo (unknown source) of all of the people who helped repair the Notre Dame cathedral. You can zoom in to see their faces.
Have a great week,
Ruth Ann Crystal MD
















.jpg)
No comments:
Post a Comment