By Katelyn Jetelina 1-6-26
"Well, he did it. He actually did it.
"RFK Jr. unilaterally made sweeping changes to the routine vaccination schedule for children in the United States. This change isn’t based on new data or new evidence, but rather on political and ideological reasons. He bypassed every scientific and clinical process we have, including not taking public comment.
"It is one of the most opaque and destabilizing public health decisions I’ve seen—it could blow up a lot of progress in childhood vaccines, which have been one of the most successful public health interventions in history. In its wake there will be confusion among parents, schools, and hospital systems, disruption of clinical workflows, possibility of increased liability, and complications with school vaccine requirements.
"The result is painfully predictable: fewer children will be vaccinated, and children will be harmed.
"This is overwhelming, but we are far from powerless. So let’s dig into: What the heck just happened? Why is this shift a problem if other countries do it? What does it mean for you? And, what can be done about it?
What the heck just happened?
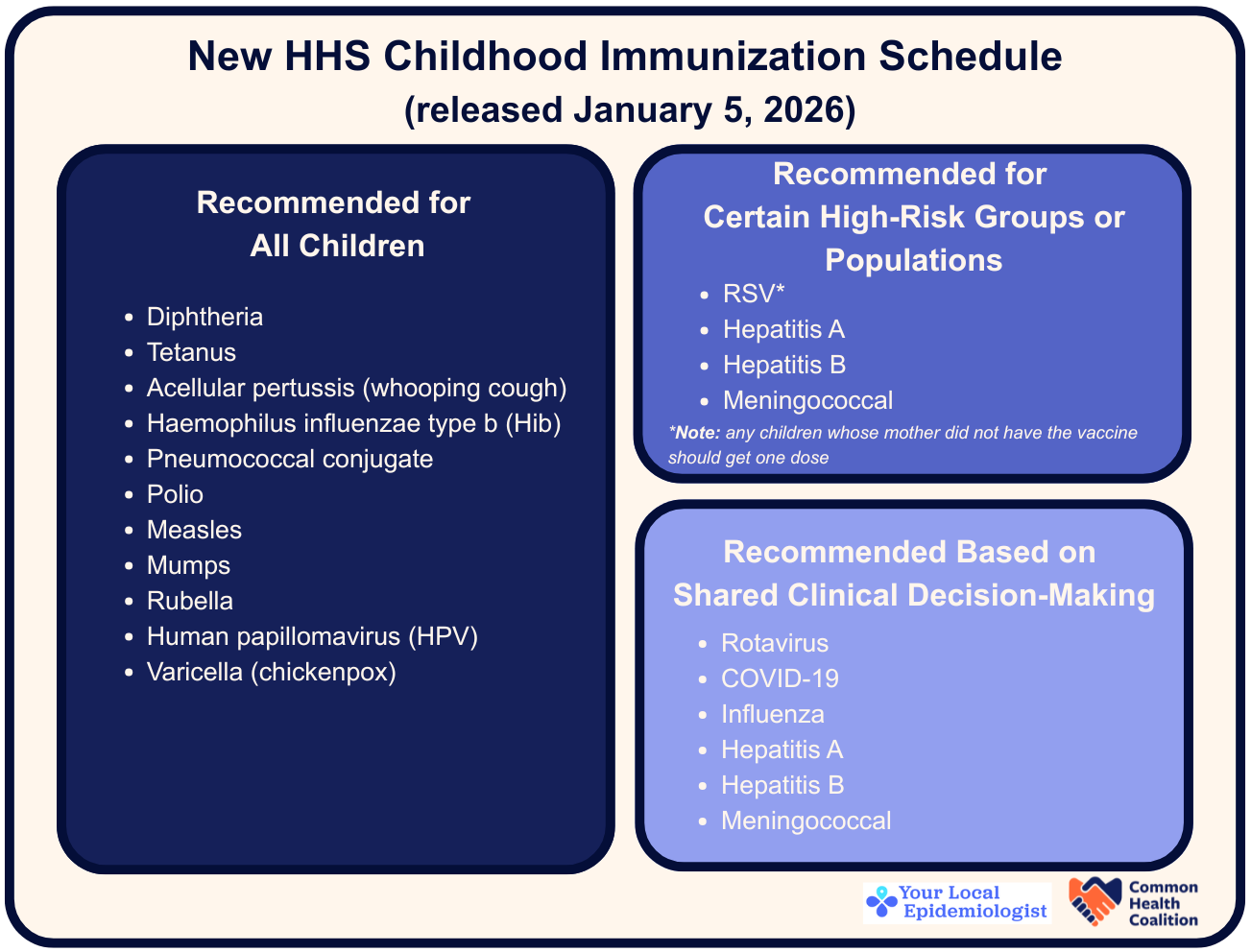
"RFK Jr. directed the CDC Acting Director to formally update the U.S. childhood immunization schedule, effective immediately, to the following:
The CDC will now routinely recommend vaccines for 11 diseases instead of 17.
Several vaccines previously recommended for all children are now:
Limited to high-risk groups.
Left to “shared clinical decision-making.”
"RFK Jr. is moving away from population-level prevention and toward individualized risk assessment. This is a fundamental shift in how the U.S. has protected vulnerable groups, how families are guided, and how parents will be asked to make decisions.
"That shift matters. A lot.
Why is this a problem? It’s like going off-roading in a Porsche
"The administration’s justification for this shift relies on comparisons to “peer countries” that recommend fewer vaccines. Denmark protects against 10 diseases, Germany 15, and Japan against 14. On the surface, this seems reasonable.
"But here’s the problem: terrain matters.
"Take Denmark. Denmark’s health and social system is well organized, well funded, and built for consistency, seamless integration for patients, and to provide a safety net for every family. Prenatal care is reliable. Nearly every child receives care on schedule. Follow-up is immaculate. And families have 46 paid weeks of maternity leave. It’s like a smooth, meticulously maintained highway where a sports car can thrive.
For example, in Denmark, only high-risk kids get the flu and Hepatitis B vaccine, and it works because of their system. Denmark screens nearly 100% of pregnant women for Hep B and follows up reliably to help prevent transmission. Medical records are also all connected, so a patient’s complete health history is always available, enabling clinicians across the system to quickly spot risks and any care gaps. Care is reliable, follow-up is consistent, and families rarely miss appointments.
"The U.S. health system is more like off-road trails in Utah. It’s fragmented, uneven, expensive, and wildly variable depending on where you live. Access depends on insurance, geography, clinic capacity, transportation, and state policy. This needs a 4-Runner built to handle potholes, steep drop-offs, and unpredictable conditions.
"Take flu and Hepatitis B, again:
For Hepatitis B, 1 in 5 pregnant women in the U.S. aren’t tested, and only 1 in 3 of those who test positive complete follow-up care. This is because care is fragmented and many don’t have prenatal care. Hep B is also often asymptomatic and poorly explained, follow-up requires extra visits, and once the baby is born the system shifts its focus away from the mother. Also, family members can give the disease to the infant. Before universal birth-dose recommendations, tens of thousands of U.S. babies fell through the cracks. There were infections each year, and 90% developed chronic infection, leading to liver failure, cancer, and early death.
For flu, families will now hear mixed messages, especially when federal leaders suggest flu shots aren’t necessary while pediatricians continue to recommend them. Some parents delay or skip vaccination. Some clinicians stop recommending it. Others soften their language, framing vaccination as optional rather than standard care. We saw this also play out years ago when the flu vaccine was recommended for only high risk. This resulted in poor coverage.
"It is beyond time we fix our roads so there are fewer health potholes in the United States. Until then, the U.S. needs a vaccine schedule designed for our messy reality. Now, we will be driving a Porsche (made for smooth roads) through those off-road trails in Utah, which is highly problematic.
"Many of the loudest arguments for simplifying schedules come from people who experience the smoothest roads: stable insurance, reliable care, and flexibility at work. But to reduce infectious diseases, public health guidance has to be built for everyone. Timing, access, and support systems are part of what make vaccines effective.
FAQ: What does this mean for you?
"We asked YLE paid subscribers what their questions were yesterday. There were a lot of good ones. Here are answers to the top 6 that we didn’t address previously in this post.
1. Can I still go to the “before” schedule?
"Yes, and you should. The American Academy of Pediatrics (AAP), which represents more than 70,000 pediatricians, still recommends the previous schedule. You can find it HERE (bookmark the page). Families can still access the full range of childhood immunizations, even if their child isn’t on the high-risk list.
2. Will insurance cover my child’s vaccines, even if they’re not on the schedule?
"Yes. The administration said that all vaccines covered by federal insurance programs—Medicaid, CHIP, and the Vaccines for Children program—remain covered. Private insurance companies have also said they will continue coverage. Whether this continues long-term is uncertain, but for now, your child’s vaccines are covered at no cost, even if your child is not high-risk.
"If this changes, hold the administration accountable.
"One exception: HPV. If your child is getting two doses, the second dose will likely not be covered under this new directive. This would be a big problem for cancer prevention.
3. Was this change legal?
"It’s a gray area. The vaccination schedule can be changed by a directive from the HHS Secretary without going to the ACIP (the external advisory committee) for a vote. Precedent for this approach was set in May 2025 with changes to the pediatric and pregnancy COVID-19 vaccine schedule.
"The legality of this action is currently under litigation by AAP. However, no injunction was issued to block implementation, meaning the revised schedule has remained in effect while the case proceeds through the courts.
4. Will health departments or NGOs be able to fill the gap?
"Nothing replaces clear, evidence-based guidance from the federal government as its reach and resources are unmatched.
"But many organizations, both new and established, have been mobilizing for the past six months—professional medical societies (AAP), coalitions, states, medical systems, and individual providers. We are trying our best to plug the holes.
5. Will this change access in the future?
"Possibly. If there is enough confusion and enough kids don’t get the vaccines, pharmaceutical companies might adjust production decisions, which could affect vaccine availability down the line. It’s also not clear how insurance coverage will play out in the long run.
6. What is shared clinical decision making (SCDM)?
"At its core, it’s a conversation about the benefits and risks of vaccines. That’s always been important, but how it’s carried out is left to the practitioner, and it can look different depending on where you go. Some clinicians may use a standard template, while others will sit down for a one-on-one discussion. In some cases, a technician will cover the basics before the pharmacist gives final approval.
"This sounds collaborative... But in practice, clinicians already do these things, and this policy signals these vaccines are now optional rather than routine. This changes how doctors counsel parents, how systems build reminders, and how families perceive importance. SCDM has historically been used for vaccines where risks could easily outweigh benefits. It was never intended to be used for widespread vaccination.
7. Why will this impact vaccination rates?
"There are myriad reasons, including:
Parents will hear that they don’t need these vaccines and so delay or skip them.
Some clinicians will stop recommending them.
Clinicians may change how they talk about vaccines.
School requirements may change to no longer require certain vaccines.
Other reasons, including hesitancy around liability among providers, supply issues because combination vaccines that include Hep B won’t work for some families, and more.
"This is going to look and feel different to everyone, but we are weakening core tenets of public health—that people should have easy, free access to vaccines, and health care practitioners should have the best information to recommend them.
What you can do
Continue to follow AAP’s vaccination schedule, not CDC’s. The AAP schedule can be found HERE.
Have questions? Chat with your pediatrician. Pediatricians know local realities of disease exposure, timing, and most importantly, your child’s medical history. Schedule conversations early, especially for children under 2.
Advocate for your state to stick with AAP guidance. Each state is responsible for the vaccination requirements for schools. Write to your representatives. Call the health department. Call your insurance company. And, send notes of encouragement if you see them sticking up for your kids. For example, I’ve already seen Maryland Health Secretary make clear recommendations.
Advocate for clear communication. If you see conflicting info from schools, clinics, or media, speak up. Encourage clear guidance.
Stay informed about disease seasons. Infections like RSV and flu have predictable patterns. Knowing when they start locally can help you plan your children’s vaccinations.
Share resources and answer questions for parents and families who are confused. There will be questions, concerns, and confusion. Lead with empathy. Be a listening ear and trusted confidant. Connect them to good resources, like AAP or YLE (shameless plug). You can use this one-pager on the vaccine changes, which we made after one YLE reader asked for it in the subscriber chat. Print, distribute, use.
Bottom line
"RFK Jr.’s CDC now recommends routine vaccination against 11 diseases instead of 17, despite no change in the underlying scientific evidence. This is a major shift that risks weakening protection against preventable diseases at a time when outbreaks are rising, and children are already being hospitalized in a health system riddled with potholes, detours, and steep drop-offs.
"AAP still recommends the previous vaccination schedule, and it remains covered at no out-of-pocket cost. What is needed most right now is clarity, answers to questions, and listening to your concerns. Demand better from those who are not acting in your family’s best interest. Don’t let confusion—or politics—take that choice away from you.
"Love, YLE'
Your Local Epidemiologist (YLE) is founded and operated by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, wife, and mom of two little girls. YLE reaches over 320,000 people in over 132 countries with one goal: “Translate” the ever-evolving public health science so that people will be well-equipped to make evidence-based decisions.













.jpg)
No comments:
Post a Comment