-----------------------------------------------
Routine vaccinations, sanitation, and a look back at history: Sanitation vs. vaccine impact, requirements, universal recommendations, Hep B and more
Katelyn Jetelina and Kristen Panthagani, MD, Ph.D - October 2, 2025
"There are many great questions—as well as confusion and doubt—swirling around routine vaccinations. We’re seeing things like: I know vaccines have saved many lives, but does everyone really need them now?
"In many ways, vaccines are victims of their success. Given the drama and polarization surrounding vaccines, it can be hard to find answers that aren’t simplistic, defensive, or angry. And, as everyone discovered during the pandemic, disease risks are often not uniform.
"Here are a few of your top questions answered!
“Did sanitation and nutrition decrease measles, or was it vaccination?”
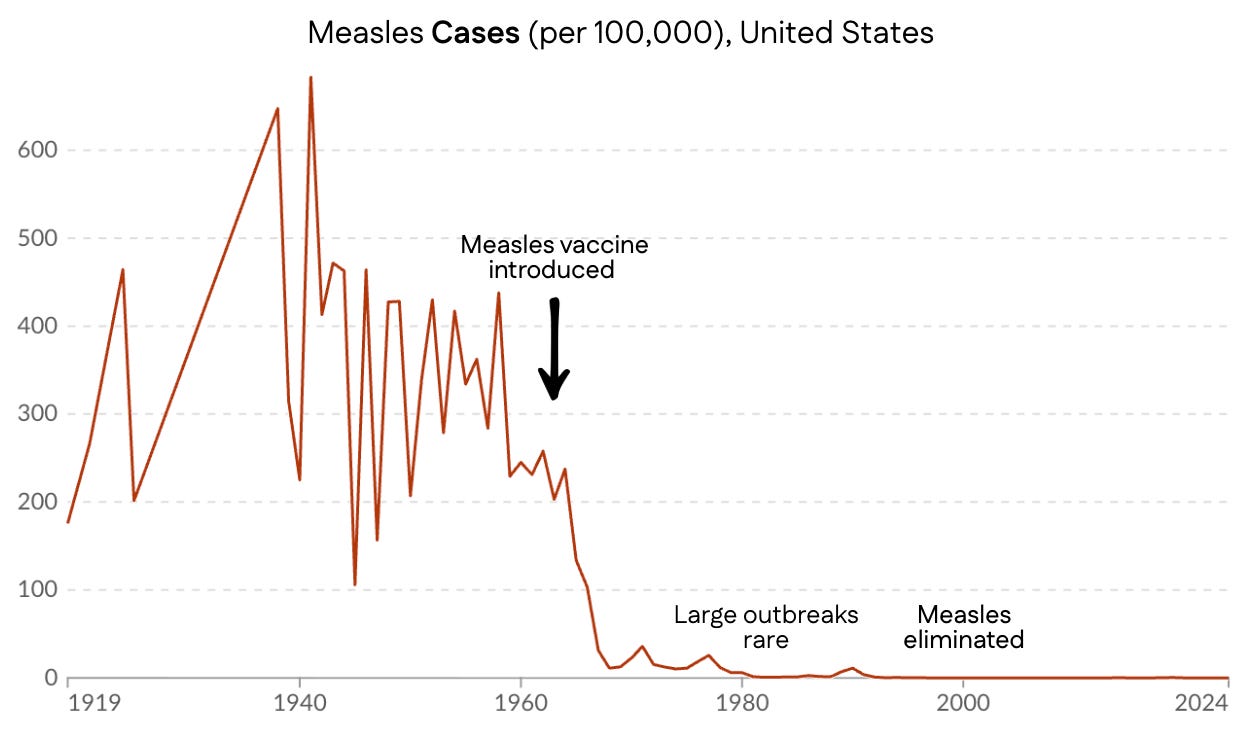
It’s true that measles deaths fell dramatically before the vaccine was introduced. Improvements in sanitation, education, nutrition, and advances in medical care made a real difference in public health over the past century, and we shouldn’t minimize that. But this graph of measles deaths alone tells only part of the story.
"While measles deaths plummeted during the first half of the 20th century before vaccination, measles infections did not. But once the measles vaccine was introduced, cases declined precipitously.
"That’s because measles is different from viruses like flu or Covid-19. The virus hasn’t changed much since the 1960s, and it replicates slowly and deep in the body. This makes the vaccine uniquely powerful: it doesn’t just reduce the risk of severe disease, but prevents infection itself.
"This is important because the infection has profound effects, even if you survive: hospitalizations, hearing loss, immune amnesia (i.e., wiping your immune system memory of all viruses), and other long-term consequences. Death is not the only outcome we want to avoid.
"We were reminded of this in a heartbreaking way just last week. A child who caught measles at 12 months old—too young to be vaccinated—died years later from SSPE, a rare but devastating brain disease caused by the virus.
"So, sanitation and nutrition did make a big impact on reducing measles mortality, but they didn’t do the whole job. When the vaccine was invented, it allowed us to eliminate measles from the U.S. Thankfully, we don’t have to choose between appreciating the historical impacts of sanitation, nutrition, and vaccination. In public health, they’re all important.
“Why are vaccines mandated for diseases that aren’t endemic, like rubella?”
"Rubella is the “R” in the MMR vaccine. It’s caused by a virus that spreads in airborne droplets from coughing or sneezing. It’s not endemic in the United States anymore. So yes, the risk is extremely low. Yet the vaccine is required for schoolchildren in all 50 states (soon to be 49 states, with news from Florida). Why?
"Think of population immunity like a dam built to prevent flooding. Once it’s built, we won’t have flooding anymore. But if the next generation comes along and says, “Hey, there’s not flooding anymore—do we really need this dam?” and decides to get rid of it, the flooding would return quickly.
"Rubella is still alive and well in other parts of the world. In the U.S., we have rubella cases yearly, but only from international travelers. However, outbreaks don’t happen often in the U.S. because population immunity—an invisible shield—stops them in their tracks. In other words, vaccination is the reason rubella isn’t endemic.
"Once a virus is eliminated from the planet and poses no risk of returning—such as smallpox—we stop vaccinating against it.
“Currently
in the U.S. the probability of getting measles is very low. If we
consider that, do the vaccine’s benefits still outweigh risks?”
"Yes, because fighting against infectious diseases is a team sport.
'Individual decisions to get vaccinated changes the risk-benefit calculation for everyone. In other words, your probability of encountering measles is low because so many people around you are vaccinated.
"But you’re right—the risk of exposure makes a difference. Let’s look at two scenarios: nobody vaccinated and everybody vaccinated. Before the measles vaccine, nearly every child in the U.S. got measles by age 15, because it’s so contagious. So risk of exposure was near 100% (to be conservative, say 95%). At 100% vaccination, the risk of measles goes to zero. Here’s what we get after accounting for exposure risk during childhood:
"Is there a situation where the probability of an individual getting a complication from measles infections roughly equals the likelihood of an adverse event from a vaccination? The math to calculate this is really tricky—it depends on not just vaccination coverage, but the risk of an outbreak, the density of the population, the size of an outbreak, etc. Even if this scenario happened, the average vaccine side effect isn’t equivalent to the average measles outcome—for example, fever-related seizures, while understandably scary to watch, fortunately often don’t require hospitalization or result in long-term problems.
"At the community level, the benefits of measles vaccination far outweigh the risks.
“Could you comment on babies getting the hep B vaccine even if they aren’t high risk?”
"The highest risk factor for Hep B (or HBV) is a history of sexually transmitted infections or multiple sex partners. So, if you’ve only had one partner for a decade, is this even applicable to your baby?
"Yes, because the hep B virus is a tricky booger:
“High risk” routes aren’t the only way of catching it. IV drug use and sexual contact aren’t the only ways hepatitis B spreads. Over a quarter of new hepatitis B cases detected in 2022 had no known risk factor or exposure. This virus is very stable in the environment (can stay infectious for days on surfaces) and only a very tiny dose is needed to cause infections (which means it can be shared through casual contact, like sharing a toothbrush).
Many people who are infected don’t know it. If we rely on moms to self-report hepatitis B infection, we will miss many cases. It’s estimated about half of people in the U.S. with hepatitis B don’t know they have it.
Screening isn’t a perfect tool. While screening moms for infection during pregnancy is highly recommended, inevitably, not every mom is screened (and some may catch it after screening), leading to missed infections. About 12% of mothers with commercial insurance and 16% of mothers with Medicaid aren’t screened appropriately, not to mention mothers who don’t have insurance for prenatal appointments.
Transmission from mom isn’t the only way babies get it. Some reports suggest that infants may catch it from other family members, such as fathers who carry the virus. Family members aren’t routinely screened, so these infections would be missed.
The outcomes can be severe. Mother-to-baby transmission at birth is the most common cause of chronic HBV infection, which can lead to liver cancer, liver failure, and death. If babies contract hepatitis B disease near birth, 95% develop the chronic form. Importantly, moving out the hepatitis B vaccine to 4 or 12 years old (instead of the historical recommendation of infants), misses the window of risk.
"The HBV vaccine induces protective immune responses in nearly everyone (80-100%). The vaccine risks are extremely low: the only safety signal found is rare allergic reactions (1 severe allergic reaction for every 2-3 million doses).
"So, all babies have been recommended to get the vaccine at birth. In the 1980s, before the universal birth dose was recommended in 1991, about 18,000 children under age 10 were infected with hepatitis B each year—half of them at birth. Today, thanks to universal vaccination, CDC reports fewer than 20 cases per year (though modeling suggests the true number is still several hundred).
“Why does the U.S. have sweeping recommendations when other countries have more targeted vaccine recommendations?”
"It’s fair to wonder why. We are all high-income countries. We all have the same vaccines. We are all looking at the same data. How could public health officials come to different conclusions across countries?
"Three main reasons:
Behavioral. Universal vaccination recommendations work better than targeted vaccinations because of convenience and increased awareness. The U.S. used to have targeted hep B vaccine recommendations, but uptake was poor. After a universal recommendation, there was a big decline in disease, and many lives (and livers) were saved. The same thing happened with the flu vaccine; universal recommendations increased uptake among high-risk groups.
Financial. Many countries’ governments pay for vaccines, so the cost-benefit analysis is a big consideration when making policy decisions. For some countries, it would be too expensive for the government to vaccinate everyone, so they try to find where the money will have the biggest impact.
Safety net. The U.S. has much less wiggle room because of worse health care access, social support, health care capacity, and health. Casting a larger net through universal vaccine recommendations is more critical than in other countries. I’ve covered this in another YLE post.
Bottom line
"The effect of vaccines is often invisible—infections prevented, childhood deaths that never happened. It’s essential to remember why we do what we do. Improved sanitation, pasteurization, nutrition, and other advances in medical care (like the development of antibiotics) also made a huge impact in reducing childhood mortality during the 20th century. Thankfully, we don’t have to choose only one!
"Thank you for your questions, and keep them coming. We’re here to answer them.
"Love, YLE and KP"
Kristen Panthagani, MD, PhD is an emergency medicine physician completing a combined residency and research fellowship focusing on health literacy and communication. She is the creator of the newsletter You Can Know Things and a regular YLE contributor. Views expressed belong to KP, not her employer.


















.jpg)
No comments:
Post a Comment